What is frontotemporal dementia? A UC Davis Health expert explains
A closer look at the disease actor Bruce Willis has been diagnosed with
After actor Bruce Willis’s family announced that he had frontotemporal dementia, many people have questions about the condition. What is it, and does it differ from dementia? For an explanation, we turned to Charles DeCarli, director of the UC Davis Health Alzheimer's Disease Research Center and distinguished professor within the Department of Neurology. In this Q&A, he addresses the neurological disorder.
What is dementia?

Dementia is not a specific disease, but rather a general term for loss of memory, language, thinking abilities and decision-making that interferes with everyday life. About 10% of adults aged 65 and older have some form of dementia.
Women are almost twice as likely than men to be diagnosed with dementia. One theory behind this is that the risk for developing dementia increases with age, and women tend to outlive men.
There are over 10 types of dementia. Frontotemporal dementia is simply one of them.
What is frontotemporal dementia?
Frontotemporal dementia (FTD) is a term that encompasses a group of brain disorders that affect the frontal (behind the forehead) and temporal (behind the ears) lobes of the brain. Over time, neurons in these regions can become damaged, which causes the brain to shrink.
FTD is the most common form of dementia for people under age 60. Unlike other types of dementia, it is as prevalent in men as it is in women.
Onset, signs and symptoms
Unlike other types of dementia, symptoms of FTD typically start in a younger age group, between 40 and 65 years old, but can also affect younger and older individuals.
Symptoms can vary widely from person to person. FTD affects the areas of the brain that are generally associated with personality, demeanor and speech. Therefore, behavioral changes in these areas are often observed first. These can include, in no particular order, changes in conduct, speech, and movement and motor skills, DeCarli said. Examples include:
- Unusual or antisocial behavior that is out of the norm for the individual
- Difficulty communicating by either being unable to speak, use and/or understand language
- Inappropriate social behavior that worsens over time
- Repetitive behavior which can include physical movements or saying the same thing over and over
- Reduced inhibitions
- Decline in personal hygiene
- Poor coordination
- Problems walking, or falling more frequently
- Muscle spasms and/or weakness
- Tremors
Risks of developing FTD
Having a family history of dementia is the only known factor, according to research, that increases the risk for developing FTD. There are no other known risk factors.
Challenges in diagnosis and importance of seeking proper treatment
Because FTD typically affects a younger age group, it can often be misdiagnosed as a psychiatric disorder such as schizophrenia, obsessive-compulsive disorder, bipolar disorder or depression. These psychiatric disorders, DeCarli explained, rarely present themselves at a later age. So, if these are being seen as new behaviors, it is particularly important to seek appropriate care from a neurological expert.

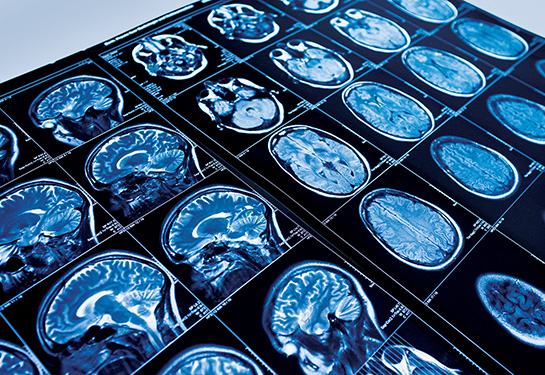
When seeking treatment, it is important for caregivers and providers to consider the patient’s mental health history. While a preliminary examination of a person with a psychiatric disorder and a person with FTD may appear similar, neuropsychological testing and brain imaging can help rule out other disorders and more accurately diagnose FTD.
Tips for families
Seeing a loved one’s behavior change can be difficult for family members. It is understandable that friends and family may become angry or frustrated as new symptoms begin to appear. As caregivers manage situations with a person who has FTD it is important to:
- Understand that the individual with FTD cannot control their behavior or symptoms, and has little to no awareness of their illness.
- People with FTD do better with routines, so creating a schedule for them is helpful.
- Simplify instructions as much as possible.
- Be patient and flexible with their changing needs and behaviors.
- Seek resources in the area.
Ask for help: Remember that self-care and outside support are crucial for caregivers to relax and recharge.
Related Resources