Rheumatology works to identify and support patients at greater risk of fragility fractures
New interdisciplinary collaboration helps prevent future fractures
As many adults age, their bodies heal more slowly, and in some cases, a broken bone could be a sign that something bigger is going on. This is especially true for the 44 million Americans who have low bone density, placing them at increased risk for fractures.
To support these patients, UC Davis Health has formed a Fragility Fracture Program, an interdisciplinary collaboration that includes the Division of Rheumatology. The goal is to ensure patients who suffer a fragility fracture receive comprehensive treatment to prevent another fracture from happening. Team members will also identify patients who might be at risk for future fractures.
A fragility fracture is a break resulting from a fall from standing height or less. These fractures, which most commonly occur at the hip, spine, or wrist, are an indication that the body’s bones have been weakened. This could indicate osteoporosis.
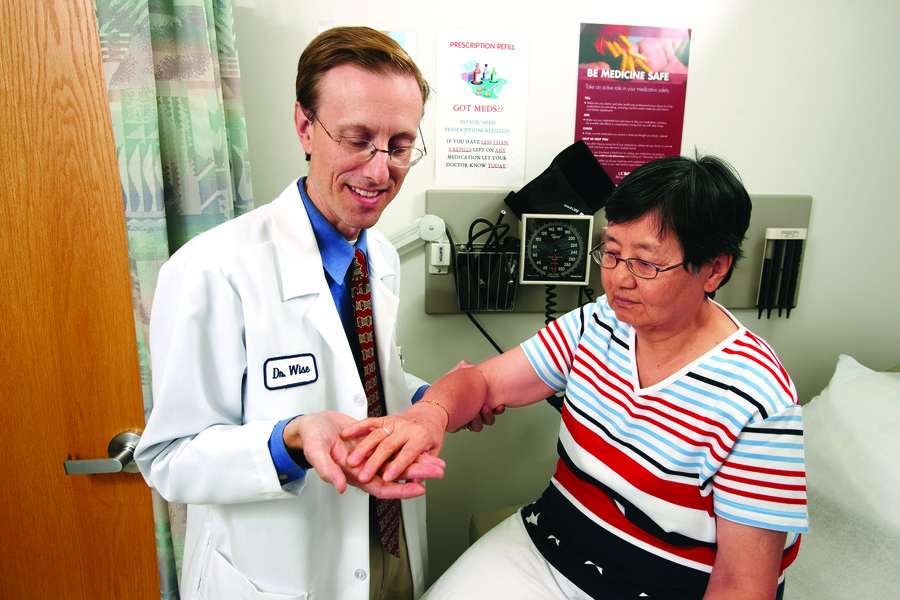
“The person at the highest risk of a fragility fracture is someone who has already had one. Second fractures can result in pain, sometimes a permanent loss of independence, and can shorten life” said Barton L. Wise, professor of rheumatology. “Yet those at risk of repeat fractures often are not referred for treatment that could prevent another fracture. Our goal is to help all of our patients regain function, avoid future fractures, and maximize their quality of life.”
Preventing future fractures
According to the National Osteoporosis Foundation, roughly half of all women and up to one-quarter of all men will suffer a fragility fracture in their lifetime. People who have had a previous fragility fracture are twice as likely to suffer a fracture in the future.
“For patients over 65, fragility fractures can lead to increased risk of mental and physical problems and a significant decrease in mobility and quality of life,” said Wise. “Some fragility fractures can be associated with a mortality rate as high as 30% within the first year.”
After a fracture, it is essential that patients be evaluated as quickly as possible for surgical intervention. Once the fracture has been managed, the immediate next step should be planning to prevent future fractures.
“When a patient experiences a fragility fracture that requires surgery it is our job to get those patients back on their feet, but we are not the experts when it comes to preventing the next fracture,” explained Hai Le, assistant professor of orthopaedic surgery. “That's when we bring in our colleagues from rheumatology and endocrinology, who are the experts in treating patients with osteoporosis or other illnesses related to low bone density.”
Finding the causes of bone fragility
Some of the critical measures rheumatology and endocrinology specialists address include laboratory testing of a patient’s vitamin D, calcium, and parathyroid and thyroid hormone levels, all of which can affect bone fragility. Other tests might be ordered as well, such as bone density measurements with DEXA scan, based on each individual patient’s needs.
“These treatments can help us manage the underlying causes of a patient’s bone fragility, so we can improve bone health and reduce risk of future fractures,” explained Wise.
Orthopaedic surgeons at UC Davis Health expressed their enthusiasm for these coordinated services to assure appropriate post-fracture follow-up.
“We are so excited to partner with rheumatology and internal medicine around this massive healthcare issue,” said R. Lor Randall, chair of orthopaedic surgery. “As our population ages, fragility fractures are affecting at least 40% of people over the age of 50, especially women. To address this challenge requires an interdisciplinary approach and this program is an example of how our surgeons are working with other experts to deliver leading-edge, value-driven, world-class care.”
Public health impact
Increased preventive treatment programs for illnesses related to osteoporosis and fragility fractures across the United States could have a major impact on public health and the high costs associated with it. The National Osteoporosis Foundation reported that approximately 1.8 million Medicare beneficiaries suffered approximately 2.1 million osteoporotic fractures in 2016.
“If we could reduce secondary fracture development by just 20%, we could potentially save Medicare over one billion dollars annually,” said Wise. “Comprehensive fracture programs could improve patient outcomes, and also provide our Medicare system additional resources to support other programs.”
