AI is on the way: Physicians enter next phase of pilot program
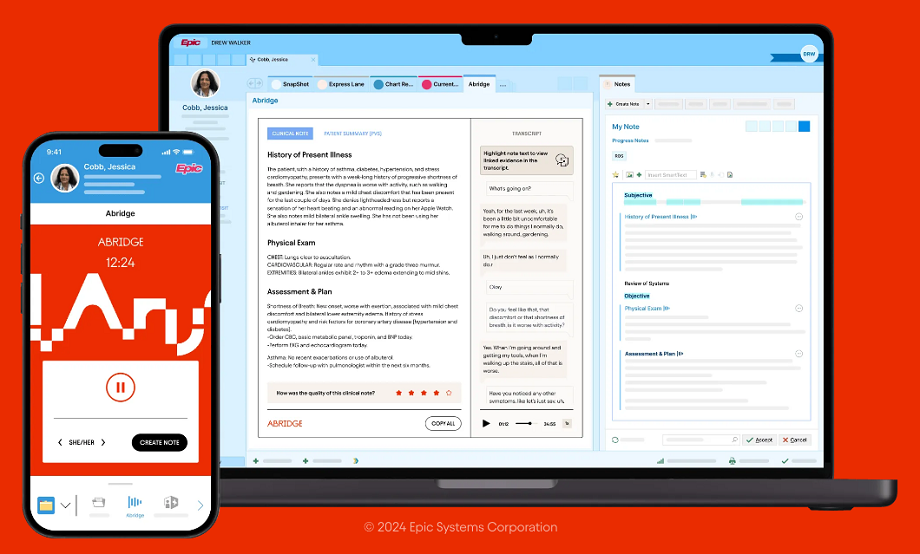
Abridge is an AI app that could help clinicians virtually eliminate notetaking
Documentation. It’s one of the most time-intensive aspects of patient care. Not to mention, note-taking during a patient visit means awkwardly turning back and forth to the computer.
AI scribe technology aims to eliminate the need for real-time notation, so clinicians can completely focus on and maintain eye contact with a patient. Following the appointment, AI organizes and structures conversation into a patient’s visit note within the Epic electronic health record (EHR). The note includes a patient-facing visit summary, assessment notes, treatment plan, physical exam and history of present illness.
It’s as simple as pressing “record.”
Between June and August, UC Davis Health will pilot the AI clinical documentation app Abridge with 27 participating physicians across internal and family medicine, pediatrics, dermatology, ENT and endocrinology.
Five physicians have already used Abridge with patients over the past several weeks, during a proof-of-concept period. Their specialties include internal and family medicine, pulmonology and critical care and gynecologic oncology.
“This technology, overnight, will revolutionize the way we see patients,” said Folsom clinic Medical Director Victor Baquero, one of the physicians testing Abridge. He demonstrated the app and shared how it has changed his practice. (The video contains sample screenshots from the Abridge app; no actual PHI is shown.)
With virtually zero editing needed, the Abridge app documents a patient summary “hands down better than the best note I can create,” said Baquero. Even when he conducted a patient interview in different languages or tried to throw off the system by discussing a health issue of a family member, the AI scribe accurately adapted the notes.
“The burden of documenting complex notes for hours each day will banish instantly. Access to care, physician burnout, accuracy of the captured information and patient satisfaction will improve as soon as we roll this out,” added Baquero.
AI technology continues to evolve and improve rapidly. In a review of 35 AI-generated transcripts, the transcripts scored an average of 48 out of 50 in key domains. Ambient scribes are being embraced by the clinical and patient communities, according to a NEJM Catalyst commentary, which also emphasized that AI is not a replacement for clinicians. All notes still require physician review for accuracy and comprehensiveness.
Though the University of California has been using forms of artificial intelligence since the 1960s, health systems around the countries are more recently piloting ambient AI technology to reduce physician burnout, improve patient access and increase face-time with patients.
It’s game-changing because for the first time in my 25-year career, I can go back to talking to the patient eye to eye and really be present."—Ashish Atreja, Chief Information Officer
“It’s game-changing because for the first time in my 25-year career, I can go back to talking to the patient eye to eye and really be present,” Chief Information Officer Ashish Atreja said in May’s Ambulatory Care Work Group. He shared that 91% of the notes so far in UC Davis Health’s pilot have been written by AI. “It should impact [physicians] in a very meaningful and positive manner in the very near future.”
Pending the success of this summer’s pilot, a phased rollout of the Abridge app will begin in the fall. The demand is already high, said Director of Clinical Informatics Melissa Jost. Physicians may need to be added to a waiting list and can reach out to her with questions.
“We are committed to finding a way to bring this across the health system to as many physicians as possible,” said Executive Director of the UC Davis Medical Group Debbie Aizenberg.
End recording.