How does obesity affect immunity, cancer and radiotherapy? It’s complicated!
UC Davis researchers hope to unlock the complex ways body fat tricks the immune system and protects tumors
Obese patients are more resistant to radiotherapy and have higher rates of cancer recurrence than other patients. UC Davis Comprehensive Cancer Center radiation oncologist Arta Monjazeb is working to find out why that is. He was recently awarded a $2.7 million 5-year grant from the National Cancer Institute for his research.
Obesity, which has reached pandemic levels in the United States, will soon surpass smoking as the number one cause of preventable cancer. That's why it has become essential to understand how to best treat obese cancer patients.
Monjazeb is collaborating with a team of UC Davis researchers to unlock the role obesity and its related hormone leptin play in radiotherapy resistance. Their studies may have major clinical implications and could help advance personalized medicine.
Personalized care for cancer patients with obesity
Monjazeb’s work focuses on understanding cancer holistically.
He says research has not paid enough attention to the patient’s metabolic profile. Monjazeb and his team are looking at how obesity impacts the radiotherapy response. They believe that what patients eat and the level of inflammation in their body may affect their cancer treatment.
“It is important to really know your patients and understand cancer in their specific context. Tailoring radiotherapy strategies to a patient's metabolic parameters can improve patient outcomes,” Monjazeb said.
Radiotherapy resistance
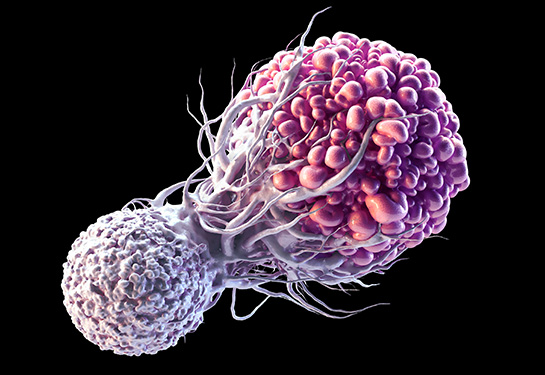
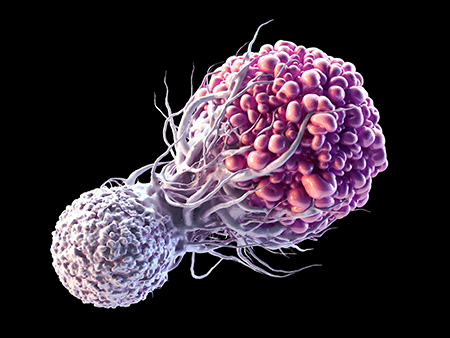
For radiotherapy to work, it needs to directly kill cancer cells and trigger the immune system to clear out the damaged cells. The success is based on its ability to cause DNA damage and kill the tumor cells as well as the immune system’s response to that damage.
Radiotherapy resistance appears when patients have less tumor shrinkage and higher cancer recurrence rates after radiation.
“Our preclinical data show increased tumor resistance to radiotherapy in obese mouse cancer models. Clinical data also demonstrate that obese cancer patients are more resistant to radiotherapy and have higher rates of cancer recurrence,” Monjazeb explained.
Unfortunately, very few studies have addressed what causes radiotherapy resistance in patients with obesity.
“Some researchers have hypothesized that this resistance is a matter of physics, as it's just harder to deliver radiation in larger patients, which may be true. But we think that there is a biological difference between cancers in obese patients and those in lean patients and the way that cancer responds to radiation,” Monjazeb added.
How does obesity affect radiotherapy?
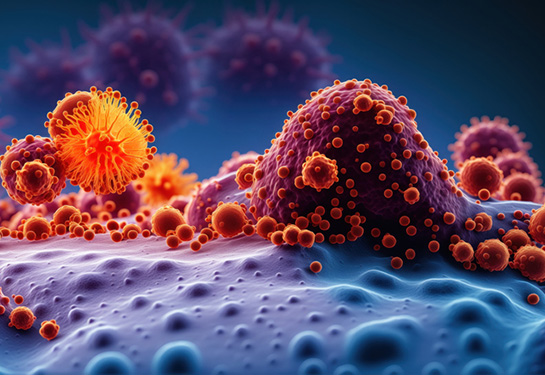
The team’s previous studies showed that obesity could alter the growth, spread and survival of cancers. They showed that the obesity-linked adipokine leptin could influence cell death and post-survival pathways of cancer cells.
Adipokines are cell-signaling molecules produced by the body’s fat tissue. They play a key role in regulating the body’s energy and metabolic status, inflammation and obesity. Leptin, a recently discovered adipokine, is highly elevated in obese patients.
We think that there is a biological difference between cancers in obese patients and those in lean patients and the way that cancer responds to radiation.” —Arta Monjazeb, UC Davis radiation oncologist
Research has shown that the immune system plays a role in how tumors react to radiotherapy. Obesity can make cancer patients more resistant to radiation by causing immune dysfunction. It may suppress the adaptive T cell response in the tumor microenvironment, impairing the immune response to cancer.
“The microenvironment surrounding the cancer cells provide nourishment for the tumor. Obesity can help feed this environment and protect the cancer cells,” said immunologist William Murphy, a co-investigator on the study. “Obesity potentially helps tumors adapt and become resistant to radiation in a nutrient rich environment. It can also result in greater inflammatory responses, allowing the cancer to spread more as well as suppress immune attack.”
Murphy is a distinguished professor and vice chair of dermatology with a joint appointment in the Department of Internal Medicine, Division of Malignant Hematology/Cellular Therapy and Transplantation.
Studying obesity’s effect on radiotherapy
The team will study the links between obesity and radiotherapy using different mouse models. They're using genetically identical mice with genetically identical tumors. The only difference is that some mice are on a high fat diet, making them gain weight. They will compare the efficacy of radiotherapy in the lean versus the obese mouse models.
They will also study radiotherapy in immunosuppressed mice to look at the direct effects of obesity on the tumor itself. The team will also evaluate how obesity and leptin signaling within cancer cells and the tumor microenvironment influence resistance to radiotherapy and immune responses.
Obesity helps tumors adapt and become resistant to radiation in a nutrient rich environment as well as potentially suppressing immune responses to the cancer.” —William Murphy, UC Davis immunologist
Future directions
In the future, they hope to study different tumor models and explore avenues to reverse radiation resistance in obese patients.
“It is possible that certain strategies that we may come up with to try to make cancers more radiation responsive will work both in obese and lean patients. These strategies may just have a more profound effect on obese patients since these mechanisms are more in play,” Monjazeb said.

Immunologist William Murphy with Logan Vick, a doctoral student and researcher at Murphy Lab
Monjazeb also received a supplemental diversity grant for $257,739 to support the work of doctoral graduate student Logan Vick. Diversity supplements provide funding to individuals from backgrounds that are generally less represented in the sciences. Vick is a researcher in Monjazeb’s and Murphy’s labs at UC Davis Medical Center.
Other collaborators on this project include radiation oncologist Jian-Jian Li, physicist Julian Perks and the Department of Radiation Oncology.
Related stories:
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.