New medical school curriculum prepares graduates to practice 21st century medicine
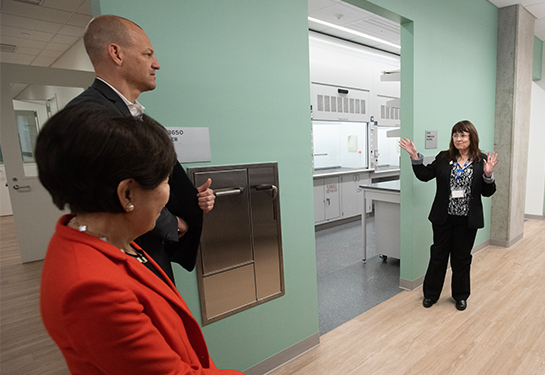
Problem-based learning groups help students take a lead role in deciding the content and direction of their learning
UC Davis School of Medicine’s innovative new curriculum is transforming the way medical students learn and prepare for careers in medicine in an ever-changing health care landscape.

The new curriculum, known as I-EXPLORE, short for Integrated Explorative Patient- and Learner-Oriented Education, was implemented for first-year medical students at the beginning of this academic year. It emphasizes cross-disciplinary collaboration and focuses on the pillars of biomedical science, clinical science and health system science.
“The I-EXPLORE curriculum is designed to prioritize collaboration, diversity, community needs, and learner-centered education resulting in patient-centered care,” said Kristin Olson, associate dean for curriculum and medical education. “Students will have the opportunity to gain knowledge, skills and experience to become the thought leaders and the change agents for the future.”
First-year medical students are currently in the pre-clerkship phase of the I-EXPLORE curriculum. That means they learn through a combination of different types of instruction with the goal of more efficient learning.
An important aspect of the pre-clerkship curriculum is the formal role of problem-based learning. During each course throughout the pre-clerkship phase, a group of 6-8 students meets three times a week with a problem-based learning facilitator.
In this group, students study a medical case, select learning objectives, identify and assess appropriate resources for relevant information, and teach one another the content. The problem-based learning facilitators help guide group sessions with the use of cases, and provide student feedback on their teamwork, communication, and critical thinking skills.
“The problem-based learning groups replicate the structure of a chief resident facilitating huddles or rounds,” explained Danielle Alexander, assistant health sciences clinical professor and problem-based learning facilitator. “This active learning approach strengthens student communication and professionalism skills they can utilize when they are residents.”
This active learning approach strengthens student communication and professionalism skills they can utilize when they are residents.” —Danielle Alexander
Each Monday, the students meet with their facilitator to identify at least eight learning objectives within a clinical case. Each student is then assigned two learning objectives to investigate on their own and present to the group in the Wednesday and Friday sessions. Students discuss the resources used and work to synthesize and reconcile the information learned. Throughout the program, the facilitator serves as a process expert rather than a content expert, thereby reinforcing the student-led nature of the learning.
“Condensing such complex issues into a four-minute presentation has really helped me learn the material better,” said Aneri Patel, first-year medical student. “I’m now able to not only better understand the concepts, but I’ve also learned how to facilitate a conversation about them.”
Over the course of the problem-based learning groups, students move through the planning, learning, assessment, and adjustment phases shown in the diagram. This evolution allows students to stretch their comfort zones, increase confidence in vocalizing their knowledge and opinions, and strengthen their ability to participate as high-functioning members of the healthcare team.
“The structure of these groups has helped reinforce the material we have learned in lecture and make us think about how to apply it to specific cases,” said Jonathan Ruiz, a first-year medical student. “It forces us to think of ways to condense the information and learn how we could share it with it a patient.”
The goals of the problem-based learning groups are to promote and practice the following foundational life-long learning skills:
- Self-directed learning emphasizes students’ self-assessment of their learning needs; their independent identification, analysis, and synthesis of relevant information; and their appraisal of the credibility of information sources.
- Independent study provides time and opportunity for student-directed learning in the core medical curriculum, based on structured learning objectives to be achieved by students with minimal faculty supervision.
- Critical judgment/critical thinking: The consideration, evaluation, and organization of evidence derived from appropriate sources and related rationales during the process of decision-making. The demonstration of critical thinking requires the following steps: A) the collection of relevant evidence, B) the evaluation of that evidence, C) the organization of that evidence, D) the presentation of appropriate evidence to support any conclusions, and E) the coherent, logical, and organized presentation of any response.
Throughout the process of problem-based learning, students also improve their skills in each domain of the UC Davis School of Medicine graduation competencies: interprofessional and communication skills, knowledge, lifelong learning, patient care, professionalism, and system-based practice.