Cerebrovascular Disease and Stroke
The UC Davis Medical Center Stroke Program features acute inpatient care as well as outpatient management of cerebrovascular disease. Patients are triaged in the Department of Emergency Medicine and receive aggressive medical care and treatment that includes:
- Thrombolytic therapy
- Interventional neuroradiologic techniques
- New medications under clinical investigation

Our inpatient stroke unit provides intense monitoring and rehabilitation of stroke patients. After discharge from the unit, patients can receive follow-up services through our weekly outpatient clinic at the UC Davis Midtown Ambulatory Care Center.
Stroke services inpatient care features a stroke unit with cardiac monitoring. Stroke services adhere to predefined admission orders for consistent, complete and efficient evaluation and treatment. Experienced neuroscience nurses staff the unit, which strives to house no more than three patients per nurse. The medical management is under the care of the stroke neurologist. Early rehabilitation is encouraged and guided by physicians from the Department of Physical Medicine and Rehabilitation. The unit also coordinates activities between nurses and therapists, including ongoing education.
Inpatient treatment:
Aggressive evaluation of stroke etiology occurs through multimodal testing with MRI, CT angiogram, catheter angiography, echocardiography, transcranial Doppler, hypercoagulable testing.
Specialized interventional treatment is available when necessary such as carotid endarterectomy, carotid stenting, intracranial artery stenting.
Intensive care unit treatment:
Where required by medical or neurological instability, patients are housed in a specialized neuroscience ICU and managed by multidisciplinary team to optimize medical and neurological treatment.
Patients developing life-threatening cerebral edema are treated by multidisciplinary team of neurologists, critical care physicians, and neurosurgeons. When appropriate, hemicraniectomy for large, space occupying strokes is available through our Department of Neurosurgery.
Inpatient ward care:
Stroke patients are assigned to specialized wards staffed by multidisciplinary teams of nurses, therapists, and physicians experienced and train specifically to care for stroke patients. Active education of patients and their families is a key component of their care. Specific measures relating to good clinical care of stroke patients is collected in a database and periodically reviewed to allow continuous improvement in quality of care. Patients receive early attention by speech therapy, occupational therapy, and physical therapy to initiate rehabilitation activities.
All stroke patients are evaluated for further subacute treatment in our specialized subacute rehabilitation wards. These wards are located directly adjacent to the acute hospital stroke wards to facilitate early evaluation and treatment by the Department of Physical Medicine and Rehabilitation.
Kwan Ng, M.D., Ph.D., Medical Director of the program along with our stroke attending physicians Kevin Keenan, M.D., Ivy Nguyen, M.D., and Alan Yee, D.O., Stroke Program Nurse Manager, the clinical stroke coordinator team, and a Stroke Program data analyst.
The team’s full complement consists of emergency medicine nurses and physicians, as well as in-house neurology residents and Neurovascular APPs.
The goal of the Acute Stroke Team is to rapidly evaluate and treat acute stroke patients, including a door-to-needle time of less than one hour for patients who are eligible for intravenous thrombolysis and identify candidates for mechanical thrombectomy who present within 24 hours of last known well, regardless of whether they receive intravenous thrombolytic therapy for the same ischemic stroke event.
Acute Ischemic stroke treatment:
- Intravenous thrombolysis within a three-hour window of last known well.
- Intravenous thrombolysis outside a three-hour window for eligible patients based on the most recent guidelines and qualified studies.
- Endovascular mechanical clot retrieval (thrombectomy) within a 24-hours of last known well is available for patients with large-vessel occlusions.
- Intra-arterial thrombolysis is available for patients who undergo mechanical thrombectomy that meet criteria determined by our stroke specialist.
Acute non-traumatic hemorrhagic stroke treatment:
- Quickly diagnosing the type and location of the hemorrhage with current imaging modalities (CT, CTA, MRI).
- Treatment may be a combination of medications or surgery with the UC Davis Department of Neurological Surgery to reduce hemorrhage expansion (blood pressure management, "blood-thinning" medication reversal), decrease brain compression, or repairing the affected blood vessels that may have caused the bleed.
The stroke service also participates in the evaluation of new forms of treatment. Examples of treatment evaluation include intra-arterial thrombolysis, mechanical clot retrieval, new methods of patient selection to extend medication time window (neuroprotectants) and surgical and medical interventions.
 Emergency Medical Services (EMS) coordinates efforts with the Department of Emergency Medicine for rapid transport of acute stroke patients. There are also ongoing educational activities for EMS and emergency department personnel.
Emergency Medical Services (EMS) coordinates efforts with the Department of Emergency Medicine for rapid transport of acute stroke patients. There are also ongoing educational activities for EMS and emergency department personnel.
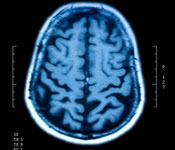
Many imaging services are available to complement stroke services. In-house computed tomography (CT) is available 24 hours per day for patients needing special care. In addition, advanced neuroimaging is routinely available for magnetic resonance imaging (MRI), resonance imaging angiography (MRA) and interventional neuroradiology.


