Research Summary
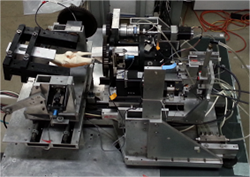
Cadaveric knee load application system
Our research develops improved surgical procedures for treating knee injury and disease with a current focus on total joint replacement primarily of the knee (TKR). More than 1 million patients undergo TKR in the US alone each year. Unfortunately, 20 – 25% of these patients have an unsatisfactory outcome due to persistent pain, instability, stiffness, and/or implant failure. These poor clinical results can be traced primarily to the conventional method for aligning the implants on the bones.
To improve clinical results, our research group pioneered a new method for aligning implants termed kinematic alignment and developed two novel surgical techniques for achieving the desired alignment. The surgical goal is to restore the alignments of the bones to the prearthritic (i.e. healthy) knee without ligament release to achieve the ultimate functional goal of restoring function to the prearthritic knee. After performing the surgery on more than 6,000 patients, clinical results as indicated by subjective patient-reported outcome scores indeed are better than those of patients who have been treated with conventional alignment methods and surgical techniques. To demonstrate the efficacy of kinematic alignment, one broad goal of our research is to conduct research projects which examine all dependent variables that provide objective measures of knee joint function for both kinematic alignment and conventional alignment methods. A second broad goal is to advance the surgical tools and/or methods to more consistently achieve the surgical alignment goals. A third broad goal is to optimize implant designs so that kinematic alignment restores knee function as closely as possible to that of the prearthritic knee.

Custom tibial force sensor
Many challenging and purposeful research projects are available which include experimental projects on cadaveric knees, experimental projects on patients both during surgery and after surgery, and computer-based projects simulating TKR on 3D bone models. Some projects involve advanced applications of biomedical imaging such as radiostereometry and fluoroscopy followed by 3D model-to-2D image registration. For the aspiring graduate student, postdoctoral fellow, or orthopaedic resident, this is an unique and timely opportunity to conduct research with immediate clinical impact which benefits the millions of patients who will undergo TKR in the coming years.
|
Anand Dhaliwal, M.D. Orthopedic Surgery Resident at Valley |
 |
|
MeiLi O’Bannon Biomedical Engineering Graduate Student |
 |
|
Ethan Bernstein Medical Student
|
 |
|
Greg Harbison, M.D. Current UC Davis Orthopaedic Surgery
|
 |
|
Deeksha Mamidi Medical Student
|
 |
|
Alexander Nedopil, M.D. Former UC Davis Orthopaedic Surgery |
 |
|
Abigail Niesen M.S., Ph.D student in Biomedical
|
 |
|
Edmond O’Donnell, M.D. Current UC Davis Orthopaedic Surgery |
 |
|
Daniel Razick Medical Student
|
 |
|
Adithya Shekhar Medical Student
|
 |
- Michelle Roland, “Virtual Axis Finder: A New Method for Finding the Rotational Axes of the Tibiofemoral Joint,” M.S. Thesis in Biomedical Engineering, 2010.
- Sue Marion, “A Mathematical Model for Fatigue of Electrically Stimulated Muscle,” Ph.D. Dissertation in Biomedical Engineering, 2010.
- Daniel Bonny, “Design, Calibration, and Validation of an Instrumented Spatial Linkage that Accurately Measures Changes in the Rotational Axes of the Tibiofemoral Joint,” M.S. Thesis in Biomedical Engineering, 2013.
- Stephanie Gu, “Simulation of Alignment Methods Used in Total Knee Arthroplasty and Their Effect on Limb and Knee Alignment,” M.S. Thesis in Biomedical Engineering, 2014.
- Josh Roth, “The Limits of Passive Motion of the Normal Tibiofemoral Joint: A Benchmark for Modeling and for Total Knee Arthroplasty,” M.S. Thesis in Biomedical Engineering, 2014.
- Abheetinder Brar, “Analysis of Reference Axes for use in Total Knee Arthroplasty Using Computer-Based Bone Models,” M.S. Thesis in Biomedical Engineering, 2015.
- Emily Meike, “Increases in Laxity Following Anterior Cruciate Ligament Reconstruction After 7 Years: An Analysis Using Roentgen Stereophotogrammetry,” M.S. Thesis in Biomedical Engineering, 2015.
- Josh Roth, “How Well Does Kinematically Aligned Total Knee Arthroplasty Prevent Clinically Important Changes in Passive Knee Function? An In Vitro Biomechanical Study of Tibiofemoral Laxities and Contact,” Ph.D. Dissertation in Biomedical Engineering, 2016.
- Jeremy Riley, “Do Varus-Valgus and Internal-External Malalignments of the Femoral Component in Kinematically Aligned Total Knee Arthroplasty Cause Clinically Important Changes in Contact Force Imbalance and Laxities of the Tibiofemoral Joint?,” M.S. Thesis in Biomedical Engineering, 2016.
- Chih Ming Hseih, “Validation of a Surgical Robot for Total Hip Replacement Surgery,” M.S. Thesis in Biomedical Engineering, 2016.
- Derrick Ross, “Validation of Tibial Contact Force Location in Single Plane Fluoroscopy,” M.S. Thesis in Biomedical Engineering, 2016.
- Stephanie Nicolet-Petersen, “Does a Posterior Cruciate-Retaining Kinematically Aligned Total Knee Arthroplasty Restore the Function of the Tibiofemoral and Patellofemoral Joints to Native? An in vivo Study of Kinematics Using Single-Plane Fluoroscopy,” M.S. Thesis in Biomedical Engineering, 2018.
- Abigail Niesen, “Computer Simulation of Errors in Migration Metrics Using Marker-Based and Model-Based Radiostereometric Analysis: Application to Risk Assessment of Tibial Baseplate Instability,” M.S. Thesis in Biomedical Engineering, 2020.
- Alexander Simileysky, “Development of Methods for Analyzing Tibiofemoral Kinematics and Contact Kinematics Using 3D Models”, M.S. Thesis in Biomedical Engineering, 2021.
- Joe Pourtabib, “Error Analysis of Methods for Determining Tibiofemoral Kinematics in the Native Knee and After Total Knee Replacement: An in vivo Study Using Single-Plane Fluoroscopy During Weight-Bearing Deep Knee Bend,” M.S. Thesis in Biomedical Engineering, 2022.
- Saul Elorza, “Tibiofemoral Kinematics of Three Tibial Insert Designs During Activities of Daily Living Following Unrestricted Kinematic Alignment Total Knee Arthroplasty," M.S. Thesis in Mechanical Engineering, 2022.
|
Societies |
|
|
Life Fellow |
American Society of Mechanical Engineers (ASME) |
|
Fellow |
Biomedical Engineering Society (BMES) |
|
Member |
Orthopedic Research Society (ORS) |
|
Member |
International Society for Technology in Arthroplasty |
|
Member |
International Radiostereometry Society |
|
Past Member |
International ACL Study Group |
|
Past Member |
American Society of Biomechanics (ASB) |
|
Past Member |
International Society of Biomechanics (ISB) |
|
Past Member |
American Society for Testing and Materials (ASTM) |
|
Past Member |
International Society for Skiing Safety (ISSS) |
|
|
|
|
Editorial Appointments |
|
|
Member |
Editorial Board, Journal of Biomechanics, 2009-present |
|
Assoc. Editor |
Journal of Biomechanical Engineering, 1998-2004 |
|
Member |
Editorial Consultants Board, Journal of Biomechanics, 1993-1999 |
|
Member |
Editorial Board, Cycling Science, 1989 - 1997 |
|
Member |
Editorial Board, International Journal of Sport Biomechanics, 1989-1992 |
|
2024 |
Major professor to Abby Niesen who won the Alan G. Marr Prize for the best Ph.D. dissertation in mathematics, engineering, and the physical sciences at UC Davis. |
|
2021 |
Robert M. Nerem Education and Mentorship Medal from the Bioengineering Division of the American Society of Mechanical Engineers |
|
2020 |
Honorary Member of the Personalized Arthroplasty Society |
|
2019 |
Coauthor on paper which received the Paolo Aglietti Award recognizing outstanding research contributing to the understanding of knee arthroplasty |
|
2012
|
Distinguished Professor, Department of Mechanical Engineering, Department of Biomedical Engineering, University of California Davis. |
|
2012
|
Creation of the Maury L. Hull Endowed Graduate Student Fellowship in the UC Davis College of Engineering with donation from Scott Maxwell |
|
2010 |
Elected as Fellow in the Biomedical Engineering Society |
|
2008 |
Bicycling Magazine Special Award for Excellence in Applied Science Research |
|
2007 |
H. R. Lissner Medal from the Bioengineering Division of the American Society of Mechanical Engineers (highest honor of the Division for career-level achievement) |
|
2005 |
Major Professor to Corey Neu, recipient of the Zuhair Munir Award for the best PhD dissertation in the College of Engineering at UC Davis |
|
2003 |
Elected as Chair of the Bioengineering Division of the American Society of Mechanical Engineers |
|
2003 |
Recipient of the UC Davis Engineering Alumni Distinguished Teaching Award |
|
2002 |
Major Professor to Tammy L. Haut Donahue, recipient of the Allen G. Marr Prize for the best PhD dissertation in the physical sciences at UC Davis |
|
1999 |
Recipient of the Best Research Paper Award from the Clinical Investigation Facility, David Grant Medical Center |
|
1998 |
Recipient of the Best Research Paper Award from the Clinical Investigation Facility, David Grant Medical Center |
|
1998 |
Recipient of the West Peak Award from the off-road bicycle industry for innovations to bicycle technology |
|
1997 |
Elected to the Executive Committee of the Bioengineering Division of ASME |
|
1993 |
Elected as Fellow in the American Society of Mechanical Engineers |
|
1989 |
Recipient of the Giovanni Borelli Award from the American Society of Biomechanics (highest honor of the Society) |
Papers Published in 2022
[1] Simileysky A, Hull ML. Repeatability, reproducibility, and agreement of three methods for finding the mechanical axis of the human tibia. Comput Methods Biomech Biomed Engin 2022;25(11):1301-9. https://doi.org/10.1080/10255842.2021.2012166.
[2] Simileysky A, Hull ML. Agreement between two methods for computing the anterior-posterior positions of native femoral condyles using three-dimensional bone models with and without articular cartilage and smoothing. J Biomech Eng 2022;144(9). https://doi.org/10.1115/1.4053914.
[3] Simileysky A, Hull ML. Can a 2D planar model more accurately determine locations of contact developed by the femoral condyles on the tibial insert in total knee arthroplasty than the penetration method? J Biomech 2022;134:110983. https://doi.org/10.1016/j.jbiomech.2022.110983.
[4] Shekhar A, Howell SM, Nedopil AJ, Hull ML. Excellent and good results treating stiffness with early and late manipulation after unrestricted caliper-verified kinematically aligned TKA. J Pers Med 2022;12(2). https://doi.org/10.3390/jpm12020304.
[5] Sappey-Marinier E, Howell SM, Nedopil AJ, Hull ML. The trochlear groove of a femoral component designed for kinematic alignment is lateral to the quadriceps line of force and better laterally covers the anterior femoral resection than a mechanical alignment design. J Pers Med 2022;12(10). https://doi.org/10.3390/jpm12101724.
[6] Niesen AE, Hull ML. Previously unrecognized source of error in the change in maximum total point motion to determine continuous migration of unstable tibial baseplates. JK Biomech Eng 2022;144(2). https://doi.org/10.1115/1.4052743.
[7] Niesen AE, Hull ML. Measurement error versus repeated measurements: a guide describing two methods for computing bias and precision of migration measurements from double examinations using radiostereometric analysis. J Biomech Eng 2022;144(6). https://doi.org/10.1115/1.4054375.
[8] Niesen AE, Garverick AL, Howell SM, Hull ML. Error in maximum total point motion of a tibial baseplate is lower with a reverse-engineered model versus a CAD model using model-based radiostereometric analysis. J Biomechanics 2022;143:111267. https://doi.org/10.1016/j.jbiomech.2022.111267.
[9] Niesen AE, Garverick AL, Howell SM, Hull ML. Low tibial baseplate migration 1 year after unrestricted kinematically aligned total knee arthroplasty using a medial conforming implant design. Knee Surg Sports Traumatol Arthrosc 2022. https://doi.org/10.1007/s00167-022-07171-4.
[10] Nedopil AJ, Zamora T, Delman C, Howell SM, Hull ML. Which asymmetric tibial component is optimally designed for calipered kinematically aligned total knee arthroplasty? J Knee Surg 2022;35(14):1610-8. https://doi.org/10.1055/s-0041-1728815.
[11] Nedopil AJ, Howell SM, Hull ML. A TKA insert with a lateral flat articular surface maximizes external and internal tibial orientations without anterior lift-off relative to low- and ultracongruent surfaces. J Pers Med 2022;12(8). https://doi.org/10.3390/jpm12081274.
[12] Nedopil AJ, Howell SM, Hull ML. Measurement of tibial orientation hhelps select the optimal insert thickness to personalize PCL tension in a medial ball-in-socket TKA. J Pers Med 2022;12(9). https://doi.org/10.3390/jpm12091427.
[13] Nedopil AJ, Dhaliwal A, Howell SM, Hull ML. A surgeon that switched to unrestricted kinematic alignment with manual instruments has a short learning curve and comparable resection accuracy and outcomes to those of an experienced surgeon. J Pers Med 2022;12(7). https://doi.org/10.3390/jpm12071152.
[14] Hull ML, Nicolet-Petersen S, Saiz A, Delman C, Howell SM. Posterior rim loading of a low-conforming tibial insert in unrestricted kinematic alignment is caused by rotational alignment of an asymmetric baseplate designed for mechanical alignment. Knee Surg Sports Traumatol Arthrosc 2022. https://doi.org/10.1007/s00167-022-06994-5.
[15] Hull ML, Howell SM. Differences in trochlear morphology from native using a femoral component interfaced with an anatomical patellar prosthesis in kinematic alignment and mechanical alignment.J Knee Surg 2022;35(6):625-33. https://doi.org/10.1055/s-0040-1716413.
[16] Hull ML. Errors in using fixed flexion facet centers to determine tibiofemoral kinematics increase fourfold for multi-radius femoral component designs with early versus late decreases in the radius of curvature. Knee 2022;35:183-91. https://doi.org/10.1016/j.knee.2022.02.011.
[17] Howell SM, Nedopil AJ, Hull ML. Negligible effect of surgeon experience on the accuracy and time to perform unrestricted caliper verified kinematically aligned TKA with manual instruments. Knee Surg Sports Traumatol Arthrosc 2022;30(9):2966-74. https://doi.org/10.1007/s00167-022-06939-y.
[18] Dhaliwal A, Zamora T, Nedopil AJ, Howell SM, Hull ML. Six commonly used postoperative radiographic alignment parameters do not predict clinical outcome scores after unrestricted caliper-verified kinematically aligned TKA. J Pers Med 2022;12(9). https://doi.org/10.3390/jpm12091468.
Papers published in 2021[1-13]
[1] Simileysky A, Ridenour D, Hull ML. Circle-based model to estimate error in using the lowest points to indicate locations of contact developed by the femoral condyles on the tibial insert in total knee arthroplasty. J Biomech 2021;120:110365. https://doi.org/10.1016/j.jbiomech.2021.110365.
[2] Shelton TJ, Gill M, Athwal G, Howell SM, Hull ML. Outcomes in patients with a calipered kinematically aligned TKA that already had a contralateral mechanically aligned TKA. J Knee Surg 2021;34(1):87-93. https://doi.org/10.1055/s-0039-1693000.
[3] Shelton TJ, Gill M, Athwal G, Howell SM, Hull ML. Revision of a medial UKA to a kinematic aligned TKA: comparison of operative complexity, postoperative alignment, and outcome scores to a primary TKA. J Knee Surg 2021;34(4):406-14. https://doi.org/10.1055/s-0039-1696734.
[5] Niesen AE, Hull ML. Propagation of registration errors into the change in maximum total point motion for determining stability of tibial baseplates. Comput Methods Biomech Biomed Engin 2021;24(9):1019-25. https://doi.org/10.1080/10255842.2020.1865324.
[6] Niesen AE, Hull ML. Propagation of registration error into maximum total point motion to analyze tibial baseplate stability at six months using marker-based and model-based RSA. J Biomech 2021;127:110651. https://doi.org/10.1016/j.jbiomech.2021.110651.
[7] Niesen AE, Garverick AL, Hull ML. Maximum total point motion of five points versus all points in assessing tibial baseplate stability. J Biomech Eng 2021;143(11). https://doi.org/10.1115/1.4051347.
[8] Nedopil AJ, Thadani PJ, McCoy TH, Howell SM, Hull ML. Adjusting insert thickness and tibial slope do not correct internal tibial rotation loss caused by PCL resection: in vitro study of a medial constraint TKA implanted with unrestricted calipered kinematic alignment. J Knee Surg 2021. https://doi.org/10.1055/s-0041-1739147.
[9] Nedopil AJ, Shekhar A, Howell SM, Hull ML. An insert with less than spherical medial conformity causes a loss of passive internal rotation after calipered kinematically aligned TKA. Arch Orthop Trauma Surg 2021;141(12):2287-94. https://doi.org/10.1007/s00402-021-04054-0.
[10] Nedopil AJ, Howell SM, Hull ML. More passive internal tibial rotation with posterior cruciate ligament retention than with excision in a medial pivot TKA implanted with unrestricted caliper verified kinematic alignment. Knee Surg Sports Traumatol Arthrosc 2021. https://doi.org/10.1007/s00167-021-06840-0.
[11] Nedopil AJ, Delman C, Howell SM, Hull ML. Restoring the Patient's Pre-arthritic posterior slope is the correct target for maximizing internal tibial rotation when implanting a PCL retaining TKA with calipered kinematic alignment. J Pers Med 2021;11(6). https://doi.org/10.3390/jpm11060516.
[12] Howell SM, Shelton TJ, Gill M, Hull ML. A cruciate-retaining implant can treat both knees of most windswept deformities when performed with calipered kinematically aligned TKA. Knee Surg Sports Traumatol Arthrosc 2021;29(2):437-45. https://doi.org/10.1007/s00167-020-05968-9.
[13] Delman CM, Ridenour D, Howell SM, Hull ML. The posterolateral upslope of a low-conforming insert blocks the medial pivot during a deep knee bend in TKA: a comparative analysis of two implants with different insert conformities. Knee Surg Sports Traumatol Arthrosc 2021. https://doi.org/10.1007/s00167-021-06668-8.



