False-positive mammogram results discourage some women from future screenings
New UC Davis study says false positives are all the more reason to keep on schedule with mammograms
Early detection of breast cancer through mammography screening continues to save lives. However, abnormal findings on mammograms can lead to women being recalled for additional imaging and biopsies, many of which turn out to be “false positives,” meaning they do not result in a cancer diagnosis. False positives can also have financial implications for patients and cause significant emotional anxiety.
A major, new study led by the UC Davis Comprehensive Cancer Center has found that women who received a false-positive result that required additional imaging or biopsy were less likely to return for that follow-up screening.
The research was published in the Annals of Internal Medicine on Sept. 3. It analyzed data on more than 3.5 million screening mammograms nationwide performed between 2005-2017 on over 1 million patients aged 40 to 73.
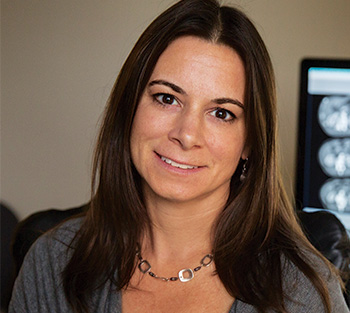
“The finding raises concerns about the potential unintended consequence of false-positive results, where women may avoid screening mammograms in the future,” said lead author Diana Miglioretti, cancer center researcher and chief of the Division of Biostatistics at UC Davis.
Findings are worrisome to researchers
The study found that 77% of women with a negative result from a mammogram returned for subsequent screening. But this percentage dropped to 61% after a false-positive finding requiring another mammogram in six months to confirm the results and 67% if a biopsy was recommended. The impact was even more pronounced for women who received false-positive results on two consecutive mammograms recommending short-interval follow-up—only 56% returned their next screening mammogram.
The high rate of women who don’t return for future screening is concerning to the research team.
“It is important for women with false-positive results to continue screening every one to two years,” Miglioretti said, “Having a false-positive result, especially if it results in a diagnosis of benign breast disease, is associated with an increased risk of being diagnosed with breast cancer in the future.”
The research also showed that Asian and Hispanic/Latinx women were the least likely to return for future screening mammograms after a false positive result, which may contribute to existing health disparities.
False-positive results are common, especially among younger women. They occur in 10-12% of mammograms in women 40-49 years of age. After 10 years of annual screenings, 50-60% of women can expect at least one false-positive and 7-12% at least one false-positive with a biopsy recommendation.
“It’s important to understand that most women recalled for additional imaging due to a finding on a screening mammogram do not have breast cancer,” Miglioretti said. “They should try not to be worried if they are recalled for additional work-up. it is a normal and common part of the screening process.”
Why do false-positive results occur?
False-positive results occur when an abnormality appears on a mammogram but further testing reveals there is no cancer. They can happen for a variety of reasons, including:
- Breast Tissue Density: Women with dense breast tissue have more fibrous and glandular tissue, which can make it more difficult to distinguish between normal and abnormal areas. Younger women are more likely to have dense breast tissue, which is the main reason why they have a higher incidence of false positives.
- Calcifications: Small calcium deposits in the breast, known as calcifications, can sometimes be mistaken for cancer on a mammogram, particularly if they appear in clusters or have certain patterns.
- Overlapping Tissue: Overlapping breast tissue can create shadows or areas that look like masses or abnormalities on a mammogram. A newer-technology, 3D mammogram reduces the chance of this happening.
- Normal variations in breast tissue: Sometimes normal variations in breast tissue look suspicious for cancer.
It is important for women to understand that about 10% of the time, additional imaging is necessary to get a better look at a finding on a screening mammogram.
Miglioretti urges physicians to carefully explain false-positive results to their patients to reassure them they don’t have cancer and stress the importance of continued screening.
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.