Engineered bone marrow shows promise as cancer treatment
Advances are revolutionizing research and treatment for osteosarcoma, the most common malignant bone cancer in children
A groundbreaking material — engineered bone marrow (eBM) — has the potential to improve treatment for osteosarcoma, a malignant bone cancer with low survival rates. A new study involving UC Davis researchers published in the Proceedings of the National Academy of Sciences describes eBM’s potential. This includes helping researchers learn how bone marrow cells affect osteosarcoma growth, testing cancer therapeutics, and potentially personalizing treatment.

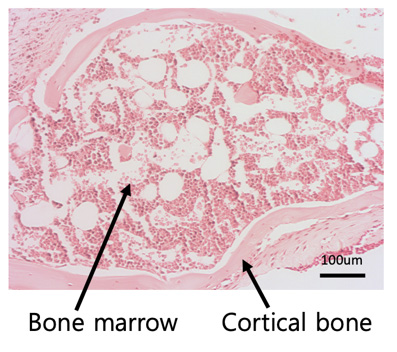
Osteosarcoma is a type of cancer that grows within bone and bone marrow. In 25% of patients, it spreads to the lungs. It’s the most common primary bone cancer in children and adolescents, usually affecting children under age 13. Survival rates are low: less than a 25% 5-year survival rate for children with metastatic cancer. Despite advancements for many other cancer types, osteosarcomes treatments have remained largely unchanged for the past four decades.
“The way we’ve previously studied osteosarcoma progression has been insufficient,” said Kent Leach, professor of Orthopaedic Surgery and Biomedical Engineering at UC Davis and the corresponding author on the paper. Leach is also the Lawrence J. Ellison Endowed Professor of Musculoskeletal Research.
Bone marrow is complex tissue with cells that can affect a tumor’s growth. However, researchers usually study osteosarcoma in flat, artificial cultures that fail to mimic the tumor environment, or mouse models with many variables that scientists can’t control. These models have limited the advancement of effective osteosarcoma treatments.
“We believe that if we can do a better job of studying how these tumor cells grow and respond to drugs, we can cut down on challenging, critical cases where tumors leave the bone, go to the lungs, and have a devastating effect on patients,” Leach explained.
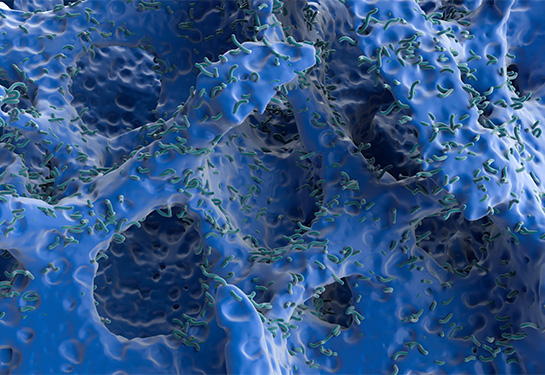
To advance osteosarcoma research and treatment, an interdisciplinary team of researchers from UC Davis and Lawrence Livermore National Laboratory developed and studied eBM. Bone marrow taken from a patient will collapse outside of the body, thereby limiting the biological relevance of the research. However, eBM maintains its integrity and provides a life-like medium to grow osteosarcoma cells. Scientists can use eBM to explore how bone marrow influences cancer growth and how osteosarcoma treatments influence cells in a realistic environment.
Multiple potential benefits of eBM
One potential use for eBM is personalized therapy for individual patients. Finding the right cancer treatment early on can lead to better patient outcomes. With eBM, there’s the potential to biopsy and culture an individual’s tumor and determine an effective treatment before starting a regimen.
“Scientifically, I’m incredibly excited,” Leach said. “I collaborate with outstanding clinicians who work every day to treat kids with osteosarcoma and other cancers that originate or metastasize to the bone. It’s a privilege to work on improved options for research with this team.”
Coauthor and Department of Orthopaedic Surgery Chair R. Lor Randall sees the exciting clinical applicability of eBM. “Engineered bone marrow maintains tremendous fidelity in creating a native microenvironment to understand how osteosarcoma develops, as well as how it behaves during metastasis to bone tissue,” he said.
Engineered bone marrow may also help improve osteosarcoma treatment for dogs. Currently, the main option for removing tumors in pets is limb amputation.
Katherine Griffin is a study coauthor and dual Doctor of Veterinary Medicine/Ph.D. candidate at UC Davis. “This work is very exciting because it lays the foundation for a technology that could be used to help veterinary and human patients alike,” Griffin said. “By providing a realistic bone marrow niche for study in the traditional lab setting, it opens doors for new discoveries.”
Other authors:
From UC Davis: Steven W. Thorpe, Thomas P. Coonan, Isabel S. Sagheb
From Lawrence Livermore Laboratory: Gabriela G. Loots, Aimy Sebastian, Nicholas R. Hum
Related Links:
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.