Orthopaedic Surgery receives over $2.2 million in research funding from defense department
UC Davis to study link between bone health and prostate cancer and prevention of arthritis after joint injuries
The UC Davis Department of Orthopaedic Surgery has received a $1.8 million U.S. Department of Defense (DOD) grant to explore how bone strength and fractures might influence the spread of prostate cancer.
It’s one of two new grants for UC Davis by the defense department.
The three-year study will investigate why prostate cancer often spreads to the bones, and whether weakened bones — due to age, fractures or hormone treatment — make patients more vulnerable to this deadly progression.
Prostate cancer is the second leading cause of cancer death in men, with one in 44 American men dying from the disease. While cancer is usually diagnosed after age 65, most lab-based research does not reflect the bone health challenges of older adults.
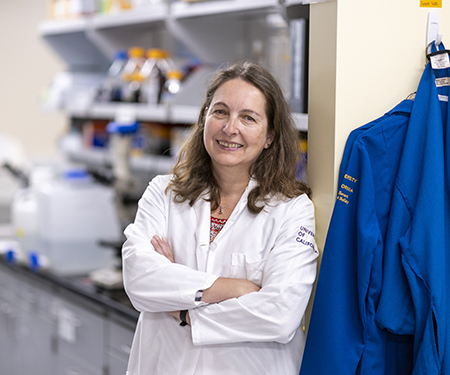
The research project is being led by UC Davis orthopaedics’ Professor Gabriela Loots, the Doris Ellison Linn Chair in Bone Biology. Co-investigators include Damian Genetos, director of Anatomy, Physiology and Cell Biology at the UC Davis School of Veterinary Medicine, and research scientist Aimy Sebastian from Lawrence Livermore National Laboratory.
"This gap in research is critical," Loots said. "Most men diagnosed with prostate cancer are older and already experiencing some degree of bone loss. That matters — especially because the cancer often spreads to the bones and becomes lethal."
Military veterans have higher rates of prostate cancer and bone injuries
A major contributor to bone loss in prostate cancer patients is androgen deprivation therapy (ADT), a common treatment that lowers testosterone levels but also weakens bones. Yet only a small fraction of men receiving this therapy undergo bone density screening, even though the risk of fracture and osteoporosis is high. This is particularly high among military veterans, who have double the rate of prostate cancer compared to civilians and face a higher risk of bone injuries.
The team plans to use mouse models that better reflect the aging human skeleton. It will test whether restoring bone density with an FDA-approved drug called romosozumab (Evenity) can prevent or slow the spread of cancer to the bones. Romosozumab is currently used to treat osteoporosis in women by stimulating new bone growth.
“If this drug can be shown to not only rebuild bone but also reduce cancer spread, it could be quickly repurposed for prostate cancer patients,” Loots explained.
This research could lead to a new approach in prostate cancer care — one that factors in bone health as a major contributor to cancer progression and uses bone-targeted therapies to protect patients from the deadliest stages of the disease.
“We are very pleased to see the recognition of this outstanding team science led by Dr. Loots,” said R. Lor Randall orthopaedic surgery chair and holder of the David Linn Endowed Chair in orthopaedic surgery. “Cancer related involvement of the skeleton makes up about 20% of the cancer care economy in the US. This project is a major step forward in helping address the medical and socioeconomic suffering of so many.”
Exploring joint damage and how it could be reversed to prevent arthritis
The second federal grant, for $442,750, is directed to the Department of Orthopaedic Surgery to investigate a little-known biological process that could help prevent post-traumatic osteoarthritis (PTOA). The painful and often disabling condition commonly develops after joint injuries such as torn ACLs or meniscus tears.
If successful, the two-year study could pave the way for new drug treatments that prevent arthritis from developing after traumatic joint injuries — a breakthrough especially important for military service members, who experience a higher rate of orthopaedic injuries.
Loots is also the lead investigator on this study, along with her colleague, co-investigator Blaine Christiansen, another professor in the Department of Orthopaedic Surgery.
“This research could have real implications for improving the quality of life for injured veterans and active-duty soldiers,” Loots said. “It’s about giving doctors tools to protect joint health before arthritis takes hold.”
Key cellular process may be to blame
The team is exploring how a recently discovered cellular process called lactylation may be at least partly to blame for joint damage and arthritis pain following injury.
Using advanced protein analysis techniques and genetically modified mice, the team will examine whether blocking the production of lactate — a compound tied to this process — can reduce joint damage and pain.
If lactylation is confirmed to be a key contributor, it could open the door to new therapies that stop arthritis before it starts.
“Right now, we have no drugs that can prevent or reverse joint damage once osteoarthritis sets in,” Loots said. “But post-traumatic arthritis gives us a unique window to intervene early — even at the time of surgery or shortly after injury.”
Osteoarthritis affects millions of people and often progresses slowly, with pain and mobility issues only surfacing once the damage is already done. For people who suffer knee injuries, such as those commonly experienced by athletes or military personnel, the risk of developing PTOA within 10–20 years is more than 50%.
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.