Air Force reservist goes to ED with stomach pain, wakes up a month and 12 surgeries later
Partnership between UC Davis Health and Travis Air Force Base helps save patient’s life
In late March, Master Sgt. Manuel Salinas started having stomach pain. He put off seeking medical care, thinking it wasn’t serious. But by March 31, the pain was bad enough that Salinas, a U.S. Air Force Reserve recruiter stationed at Travis Air Force Base, went to David Grant Medical Center. Little did he know that he would spend the next 50 days in the hospital undergoing 12 lifesaving surgeries.

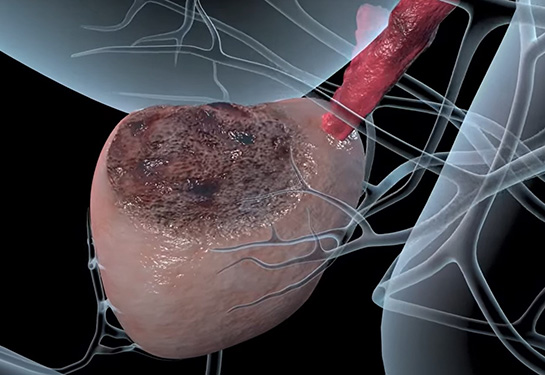
Salinas suffers from hypertriglyceridemia, a condition that causes high levels of triglycerides – a type of fat – in the blood. People with this ailment have an increased risk of acute pancreatitis – a condition where the pancreas becomes swollen over a short period of time. Salinas thought his stomach pain was probably caused by pancreatitis due to the hypertriglyceridemia.
“I’ve had pancreatitis before, and it felt like I had pancreatitis again,” Salinas said. “But while I was there, I told the doctor, ‘Hey, I think this might be something more than just pancreatitis because the pain is migrating to other parts of my abdomen.’”
A CT scan quickly revealed that it was a reoccurrence of acute pancreatitis. Most people with acute pancreatitis fully recover. But for patients with hypertriglyceridemia, like Salinas, it can be much more serious. As acute pancreatitis progresses, blood pressure drops as the body focuses on keeping the brain and heart alive by constricting blood flow to other organs.
Such was the case with Salinas. His organs began shutting down, starting with his kidneys. Within 24 hours, he was fading in and out of consciousness. His doctors recommended he be transferred via helicopter to UC Davis Medical Center to receive specialized care. Salinas remembers waking up momentarily in what he describes as a “vessel of some sort” before losing consciousness again.
“I remember seeing people with helmets on, and you know, the inside of a spaceship is what I thought I remembered,” recalled Salinas with a chuckle. “I remember somebody lifting a plastic safety button, hitting the red button and us taking off.”
The surgeon on call in the Department of Emergency Medicine that night was Rachel Russo, an assistant professor in the Department of Surgery and a Major in the U.S. Air Force.
“When he came in, his systolic blood pressure was in the 50s,” Russo said. “They were minutes from starting chest compressions on him. I immediately recognized that he needed emergency surgery and would be too sick to transfer to the operating room.”
UC Davis Health staff immediately gathered the necessary equipment to operate in the ICU – an unusual event. This included stools to stand on to accommodate for the higher, wider beds, headlamps to increase visibility and handheld tools that are normally integrated into standard operating rooms.
When he came in, his systolic blood pressure was in the 50s. They were minutes from starting chest compressions on him. I immediately recognized that he needed emergency surgery and would be too sick to transfer to the operating room.” —Rachel Russo
Russo’s military experience and participation in the 30- year civilian-military partnership between UC Davis and David Grant Medical Center played a role in her readiness to adapt to the challenging circumstances. She, along with some members of the surgical team – other current and former members of the military – brought with them unique knowledge from combat surgery, enhancing their approach to Salinas’ deteriorating condition.
12 life-saving surgeries
That night, Russo performed three surgeries on Salinas to remove parts of his bowels which had become necrotic and were dying, due to his failing organs. She made an incision from the bottom of Salinas’ sternum to the top of his pubic bone and removed his colon. He needed multiple blood transfusions, blood pressure medication, and intubation to help him breathe.

“When Dr. Russo called the night of the 2nd of April, she was pretty clear that he was very critical,” recalled Cassandra Casul, Salinas’ best friend, who was stationed at Tinker Air Force Base in Oklahoma at the time. “She told his father and me that she did not think he was going to make it through the night.”
Against the odds, Salinas survived the night. His condition improved slowly, and he remained in a coma for about a month, due to sedation and the trauma his body had endured. During that time, UC Davis Health surgeons performed several additional surgeries to his abdomen to remove more necrotic tissue.
When Dr. Russo called the night of the 2nd of April, she was pretty clear that he was very critical. She told his father and me that she did not think he was going to make it through the night.”—Cassandra Casul
Waking up from a month-long coma
On April 28, 2022, Salinas awoke fully from the coma. It was a shock.
“I was like, ‘What!? Three weeks? Four weeks? What are you talking about?’”
Salinas remained in the hospital for another three weeks. After learning more about his condition, how close he had come to death, and seeing photos of himself while in a coma, Salinas experienced a form of post-traumatic stress disorder. He was placed on antidepressants and anti-anxiety medication.
Still, he feared being alone in the recovery room. He did not want the lights off, the door or curtains closed, nor did he want to fall asleep. He insisted on keeping the call button close, so much so that he could not fall asleep without it on his chest.
Casul stayed on the phone with him for hours, assuring him whenever he woke that he was alive and no longer in imminent danger.
I was like, ‘What!? Three weeks? Four weeks? What are you talking about?’” —U.S. Air Force MSgt. Salinas
A long road to recovery
Salinas is still on the road to recovery. Once a robust man, he has lost much of his overall physical strength. He had to learn to swallow again, to pick up utensils and feed himself, and had difficulty talking clearly due to a tracheotomy that had been performed while in a coma. He also struggled to use a keyboard or to write.

“There is a picture where I was trying to write,” Salinas described. “It literally looks worse than a kindergarten kid. They were more like figures as opposed to letters. It was so, so frustrating.”
Salinas underwent a total of 12 surgeries while at UC Davis Medical Center. He returned nearly two months after discharge for a 13th surgery, when surgeons were finally able to close the incisions made during his initial bowel surgeries. Russo said they used a mesh, specialized dressings and skin grafting on top of his bowels.
“Salinas was aided by civilian and military personnel sharing their expertise,” Russo explained. “These were skills brought back from wartime care.”
Now at home, he relies heavily on support from his father, Manuel Salinas Sr., who visits him frequently and provides physical and emotional support. Salinas still has an ileostomy bag, (a bag attached to an opening near the abdomen so that stool can be collected outside the body).
He still needs one more surgery to remove the ileostomy bag and reconstruct his bowels. He is not ready to retire, even after more than 20 years of military service.
He’s grateful for the care he received at both Travis Air Force Base and UC Davis Medical Center, and attributes his survival to the expert coordination between the two medical teams.
When asked about the care he received at UC Davis Medical Center, Salinas and his best friend Casul simultaneously exclaimed that it was “Amazing!”
“Dr. Russo’s team on the night of the 2nd of April, they saved his life. He was minutes from death but that initial surgery saved his life,” Casul said.
UC Davis Health and David Grant Medical Center have partnered successfully for over thirty years. Through this civilian-military program, military surgical residents gain exposure to trauma care by working alongside experienced UC Davis Health physicians. Likewise, military physicians and surgeons who return from deployment work at UC Davis Medical Center, bringing unique knowledge from combat surgery which they pass on to civilian clinical personnel through teaching and mentorship.