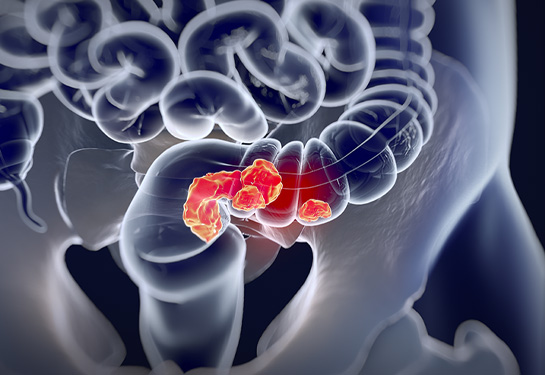
Colon and rectal cancer on the rise in young adults
Surgeons advise “putting down the knife” when treating rectal cancer
Millennials beware: Your chance of getting colon cancer has gone up!
Colorectal cancer is now the No. 1 cause of cancer death for men under 50 and the No. 2 cause of cancer death in women in that age group.
That was news to a 40-year-old mother of three. Kasey (who asked to be identified only by her first name) took an at-home colorectal cancer detection kit that indicated she didn’t have cancer. But she sensed something was off. So, after several trips to the doctor in 2022, and a long wait to schedule a colonoscopy, and then a further round of scans, she finally learned she had stage 3 rectal cancer.
“My husband and I were in shock,” Kasey said.
Treatment began immediately
Experts from the UC Davis Comprehensive Cancer Center told Kasey that the best approach to her treatment would be to start with four months of chemotherapy overseen by medical oncologist Rashmi Verma, followed by six weeks of radiation, overseen by radiation oncologist Arta Monjazeb.
At the end of treatment, she received the welcome news that her tumor appeared to have completely gone away and she wouldn’t need surgery. Instead, her colorectal surgeon Ankit Sarin placed her on a close-monitoring protocol called “watch and wait.”
“We have seen a significant change in the management of rectal cancer in the last decade and in a proportion of these patients, putting down the knife is the best thing a surgeon can do,” said Ankit Sarin, chief of the Division of Colorectal Surgery.
Sarin added, “We were able to offer Kasey this partly because, as the only nationally accredited program for rectal cancer in the region, our team of multidisciplinary doctors review and follow each patient with rectal cancer using strict accreditation standards, and each patient gets chemotherapy, radiation and, or, surgery specifically tailored for them."
Surgery of the rectum sometimes means the patient must have an ostomy. Whether temporary or permanent, it can have a major impact on their quality of life.
“We are constantly adapting our care based on emerging evidence,” Sarin said. “Shifting chemotherapy to before surgery, adding immunotherapy in select patients and using cell-free DNA technology are all part of this new approach.”
Verma added that, in contrast to rectal cancer, most patients with localized colon cancer require surgery first, followed by chemotherapy or immunotherapy, depending on the tumor/cancer type and extent of the cancer spread.
Colorectal cancer is challenging to diagnose
Oncologists worry that symptoms in young adults are often brushed off.
“Primary care doctors don’t think of colorectal cancer in younger patients who are commonly diagnosed instead with inflammatory bowel disease,” said Verma. “If an at-home test is prescribed and results come back negative, but symptoms continue, tell your doctor you want a colonoscopy.”
Along with raising children who, at the time, were 2, 5 and 7 years old, Kasey kept to a healthy diet and an exercise routine, which included yoga, running and hiking.
“If colorectal cancer can happen to me, it can happen to anyone.” Kasey said, adding that there is no history of colorectal cancer in her family.
Unrelenting symptoms
Kasey has a clear memory of her symptoms. “I knew something was wrong,” Kasey said. “I had the need for bowel movements frequently, perhaps as many as 10 times a day, blood was present and there was pain in the region.”
Verma explained that because the rectum is in the lower part of the colon, patients feel more urgency and pressure in the rectal area as well as soreness. In comparison, colon cancer symptoms usually include abdominal pain, weight loss and bowel obstruction. Most colorectal cancers, however, are asymptomatic, which is why screening is so important.
Kasey said the soreness continued to worsen. At first, her primary doctor thought she had irritable bowel syndrome or internal hemorrhoids, but when her pain intensified, she became convinced she needed to insist on answers.
“If your symptoms don’t stop, don’t give up. You are your own best advocate,” Kasey said.
Troubling trend
People born between 1981 and 1996 face twice the risk of colorectal cancer as those born in 1950.
As a result of this troubling trend, the U.S. Preventive Services Task Force changed its recommendations in 2021 for people to begin getting colon cancer screenings at age 45 — instead of the previously recommended age of 50.
Experts aren’t sure why there’s an increase in young adults getting colon and rectal cancer. Researchers are exploring factors such as diet, obesity, lack of exercise, tobacco and alcohol use as well as environmental impacts such as exposure to chemicals. Family history also plays a role.
Kasey said she was able to cope with treatment without taking much time off from work. She also didn’t experience hair loss and felt the energy to keep up with her kids, which she thinks made her cancer treatment less stressful on the family.
“I am so thankful for my colorectal cancer team at UC Davis,” Kasey said. “Dr. Verma, Dr. Monjazeb and Dr. Sarin provided terrific care and I’m grateful the treatment has been successful.”