Could a new medical approach fix faulty genes before birth?
A new study in mice shows a unique mRNA delivery method for in-utero gene editing for neurodevelopmental conditions
A new study shows that a biomedical tool can successfully deliver genetic material to edit faulty genes in developing fetal brain cells. The technology, tested in mice, might have the potential to stop the progression of genetic-based neurodevelopmental conditions, such as Angelman syndrome and Rett syndrome before birth.
"The implications of this tool for treating neurodevelopmental conditions are profound. We can potentially correct genetic anomalies at a foundational level during critical periods of brain development," said the study’s senior author Aijun Wang, a UC Davis professor of surgery and biomedical engineering.
The study, a collaboration between the Wang Lab and the Murthy Lab at UC Berkeley, was published today in ACS Nano. The team hopes to develop this technology into treatments for genetic conditions that can be diagnosed during prenatal testing. The treatments can be given in the womb to avoid more damage as cells develop and mature.
The implications of this tool for treating neurodevelopmental conditions are profound. We can potentially correct genetic anomalies at a foundational level during critical periods of brain development,"—Aijun Wang, professor of surgery and biomedical engineering
A complex transportation system with a revolutionary delivery method
Proteins have a crucial role in the way our bodies function. They are assembled in cells based on instructions from messenger RNA (mRNA). In certain genetic conditions, the genes express (produce) more or fewer protein than the body needs. In such cases, the body might get dysregulated and need to silence an overactive gene or supplement the low protein levels.
“Proteins have large and complex structures, which makes them hard to deliver,” Wang said. “Their delivery remains a huge challenge and a dream for treating diseases.”
Instead of delivering proteins, scientists found a way to deliver mRNA to cells that will be translated to functional proteins within the cells. This delivery method uses a unique lipid nanoparticle (LNP) formulation to carry mRNA. The objective is to introduce (transfect) mRNA genetic material into the cells. The mRNA then would translate instructions to build proteins.
Delivery of mRNA using LNP is already transforming disease treatments. It has applications in vaccine development, gene editing and protein replacement therapy. Recently, mRNA delivery became more popular with its use in Pfizer and Moderna COVID-19 vaccines.
Importance of efficiency in LNP delivery of mRNA
In a recent Nature Nanotechnology paper, Wang, Murthy and their team described a new LNP formulation to safely and efficiently deliver mRNA. LNPs carrying mRNA need to arrive at the cells, where they will be taken in through a process known as endocytosis. There, the cell breaks the LNP carrier, which allows the mRNA cargo to be released.
One mRNA is around 100 nanometers in size. For comparison, a sheet of paper is about 100,000 nanometers thick.
“The LNPs developed in this study use a new acid degradable linker that enables the LNPs to rapidly degrade inside of cells. The new linker also enables LNPs to be engineered to have lower toxicity,” said Niren Murthy, professor of bioengineering at the University of California at Berkeley and co-investigator on this project.
“When the cells uptake the LNPs, the particles get degraded in the acidic environment of the cell’s endosome. This causes a more efficient and early release of mRNA to the cytosol, the liquid component inside the cell where the mRNA will be translated into proteins. That is where we want to have the mRNA to be effective and functional,” Wang explained.
Efficiency is closely linked to toxicity. For this reason, it is important to know the number of LNP carriers a cell needs to uptake to make enough proteins. If the uptake efficiency is low, scientists will need to use a lot of nanoparticles. This means multiple doses or high doses that can cause a toxic immune response.
“The biggest hurdle to deliver mRNA to the central nervous system so far has been toxicity that leads to inflammation,” Wang said.
The study showed that the LNP method is more efficient at mRNA translation, reducing the need for potentially toxic doses.
Sending the manual to build the CAS9 enzyme for gene editing
The new study describes the use of the LNP technology for Cas9 mRNA delivery to treat central nervous system genetic diseases in utero. The researchers tested their tool on the gene responsible for Angelman syndrome, a rare neurodevelopmental condition.
In a genetic condition, damage accumulates during gestation and soon after birth. Research shows that it is more efficient to deliver therapies to the brain cells before the blood-brain barrier in babies is fully formed. So, the earlier the correction happens, the better. The idea was to stop the disease progression in-utero.
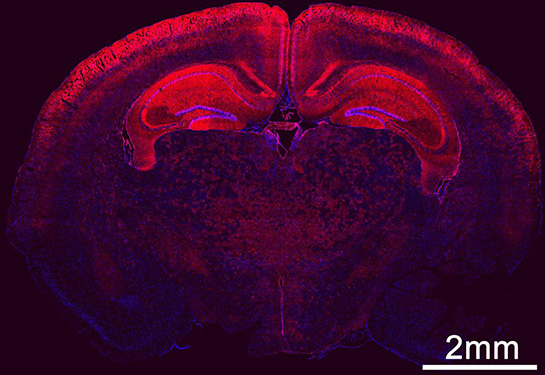
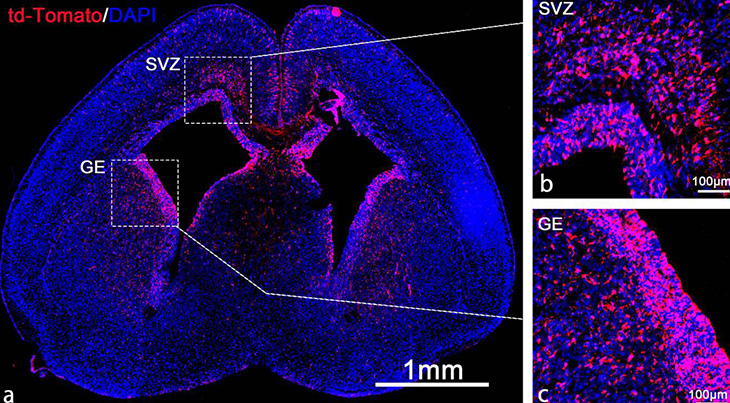
The researchers injected the LNP with the mRNA into the fetal brain's ventricles in a mouse model. The mRNA translates into CAS9, a protein that works like scissors for gene editing. The produced CAS9 will edit the gene responsible for Angelman syndrome.
“The mRNA is like the Lego manual that has instructions to put the pieces together to form functional proteins. The cell itself has all the pieces to build CAS9. We just have to supply the mRNA sequence, and the cell will take and translate it into proteins,” Wang explained.
The mRNA is like the Lego manual that has instructions to put the pieces together to form functional proteins. The cell itself has all the pieces to build CAS9,” —Aijun Wang, professor of surgery and biomedical engineering
Findings
The study showed that the LNP tool was very efficient in delivering the mRNA that translated into CAS 9.
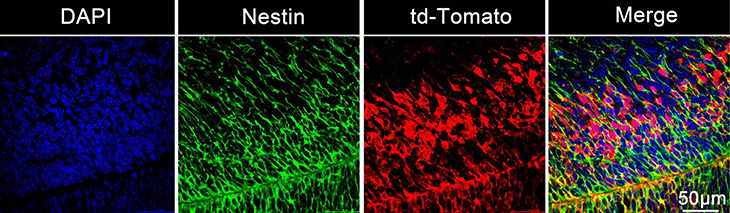
Using tracers, the researchers could see all the neurons that were edited inside the brain. Their study showed that the nanoparticles were taken up by the brain’s developing neural stem and progenitor cells. The nanoparticles led to gene edits in 30% of the brain stem cells in the mouse model.
“Transfecting 30% of the whole brain, especially the stem cells, is a big deal. These cells migrate and spread to many places across the brain as the fetus further develops,” Wang said.
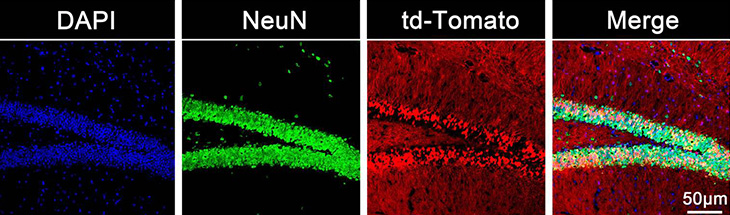
In the study, as the fetal development continued, the stem cells proliferated and migrated to form the central nervous system. The study revealed that more than 60% of the neurons in the hippocampus and 40% of neurons in the cortex were transfected.
“This is a very promising method for genetic conditions affecting the central nervous system. When the babies are born, many of the neurons could have been corrected. This means the baby could be born with no symptoms,” Wang explained.
Wang expects to see an even higher percentage of transfected cells in a diseased mouse model.
“Bad neurons with mutation may be killed by the accumulation of disease symptoms and good neurons may stay and proliferate. This could lead to amplified therapeutic efficiency. If we know well enough how cells work, we can leverage this knowledge to cooperate with the naturally occurring pathways in the cell,” he said.
Collaboration with MIND Institute and UC Davis Institute for Regenerative Cures
Wang is the vice chair for translational research, innovation and entrepreneurship at the Department of Surgery and co-directs the Center for Surgical Bioengineering at UC Davis. His work is built on a strong collaboration with Murthy lab at UC Berkeley and partnerships with many UC Davis researchers.
“We at UC Davis are so well and uniquely positioned. We have a great Fetal Treatment Center under the leadership of Dr. Diana Farmer and Dr. Shin Hirose, and the Institute of Regenerative Cures, led by Dr. Jan Nolta,” Wang said.
Currently, his team is working with the UC Davis MIND Institute’s Jill Silverman, who is a professor in the Department of Psychiatry and Behavioral Sciences, to use LNP technology for Angelman syndrome research. Together, they hope to test LNPs in mouse models of various neurological diseases. At a later stage, they will explore the success of this tool in large animal models before human clinical trials.
The study was supported by Shriners Children’s research grant 85400-NCA-24 and National Institutes of Health (NIH) grants 1R01NS131538-01A1, R01MH125979-01 and 1R21NS133881-01. It was also funded by the California Institute for Regenerative Medicine (CIRM) DISC2-14097 and DISC2-14045, the Innovative Genomics Institute and the CRISPR Cures for Cancer Initiative.
UC Davis coauthors are Diana Farmer, Matileen Cranick, Shanxiu Xu, Boyan Yin, Hengyue Song, Maria Clarke, Kewa Gao, David Wang, Jessica M. Wong and Zehua Zhao. Farmer is also affiliated with Shriners Hospitals for Children, Yin with UC Berkeley, and Song with Central South University. Coauthors from UC Berkeley are Hesong Han, Sheng Zha and Benjamin W. Burgstone. Coauthor Yibo Hu is at Central South University.