New study confirms community pharmacies can help people quit smoking
Pharmacists may play crucial role in addressing lack of access to tobacco cessation tools
A new study shows community pharmacies may play a key role in helping people quit smoking.
The findings came out in the article Closing the Tobacco Treatment Gap, published in the 10th anniversary special issue of Pharmacy. The results provide valuable insights into the implementation of tobacco cessation services within community pharmacies while identifying barriers to further improvements.
Tobacco use remains a leading preventable cause of death. Although two thirds of people who smoke would like to quit, many individuals trying to quit on their own are not successful. To address this gap, the study explored how pharmacists and pharmacy technicians could assist in providing tobacco cessation support.
Led by researchers at UC Davis Comprehensive Cancer Center and other academic institutions across the country, the study involved seven independent community pharmacies in California affiliated with the Community Pharmacy Enhanced Services Network. A total of 22 California pharmacists and 26 pharmacy technicians who underwent tobacco cessation training participated.
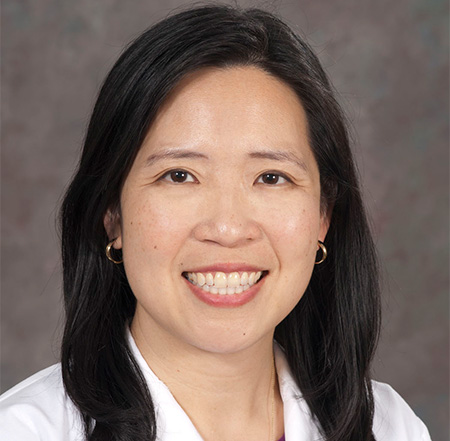
“Community pharmacies are important partners to expand access to tobacco cessation services,” said Elisa Tong, a UC Davis Health internist and director of the cancer center’s Tobacco Cessation Policy Research Center. “By state law, pharmacists can furnish all forms of nicotine replacement therapy (NRT) without a provider prescription.”
California’s law allowing pharmacists to provide the cessation tool took effect in 2014. Eligible pharmacists must complete two hours of tobacco training and follow the state-approved protocol, which consists of reviewing patients’ current tobacco use and prior quit attempts, screening for appropriateness of NRT, providing medication counseling, and addressing or referring patients for behavioral counseling. Tobacco cessation has been integrated into the curricula of California pharmacy schools since 2000, and many other training programs are available for pharmacies.
“After completing tobacco treatment training, our research showed that pharmacies successfully initiated cessation services,” said the study’s senior author Karen Hudmon from Purdue University College of Pharmacy. “Compatibility with existing workflows, staff buy-in and the crucial role of pharmacy technicians significantly helped.”
Continued research efforts are underway to study policy implementation strategies, especially for pharmacist reimbursement. California’s law authorizes Medi-Cal and private insurance to pay pharmacies for enhanced services including education and medication management.
“Pharmacists and pharmacy technicians play a pivotal role in providing effective support for tobacco treatment and other related health issues,” said Robin Corelli, a UC San Francisco pharmacy faculty member and study co-author. “Being part of the local community is important and we need sustainable models for providing these services.”
Solving barriers could help pharmacies reach more people
Given that 89% of Americans live within five miles of a community pharmacy, they can be convenient locations for receiving health care services. Pharmacists have shown to be effective in helping patients quit. They can reach uninsured and under-resourced patients as well as patients living in rural areas who might experience barriers to accessing primary care. However, the study showed certain barriers exist to making pharmacy cessation programs effective.
The research showed that billing complexities, software limitations and training gaps for handling complicated patient cases all pose challenges to successful implementation of tobacco cessation services at pharmacies.
However, the data collected implied a forward-thinking health care model where the pharmacists and their staff can play a fundamental and dynamic role in local health management, and ultimately, in cultivating a healthier population. The study serves as a valuable resource for policymakers, health care professionals and stakeholders in population health efforts to combat tobacco use.
This study was funded by the National Cancer Institute (R25 CA236637 to K Hudmon) and the Tobacco-Related Disease Research Program, which also supports the Tobacco Cessation Policy Research Center at UC Davis Comprehensive Cancer Center.
The cancer center’s new Tobacco Cessation Policy Research Center will continue to examine the role of pharmacies in helping people quit smoking. The center is also studying the integration of tobacco treatment at substance use disorder facilities. Other tobacco-related research focuses on equal access to tobacco treatment provided by public insurance plans and engaging with enforcement of flavored tobacco sales restrictions.
Other authors include:
Katy Ellis Hilts of Richard M. Fairbanks School of Public Health at Indiana University; Nervana Elkhadragy of University of Wyoming School of Pharmacy; Micah Hata of College of Pharmacy, Western University of Health Sciences, Pomona; and Francis M. Vitale of College of Pharmacy, Purdue University.
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.