UC Davis Health surgeons use FLIm imaging to detect head and neck cancer during surgery
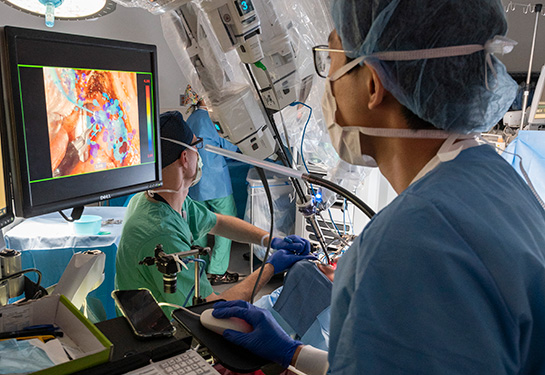
A UC Davis Health team of surgeons and scientists has integrated a novel imaging technology with robotic surgical systems to help detect primary cancerous tissue during head and neck cancer surgeries. The technology, known as Fluorescence Lifetime Imaging (FLIm), allows surgeons to identify and remove malignant primary tumors more precisely and thoroughly.
Primary tumors are cells where the cancer first starts. It is important to locate these tumors for appropriate treatment and to improve the chance for cure.
In a study published in Head and Neck journal, the team shared the results of testing FLIm in six patients with squamous cell carcinoma of unknown primary in the head and neck.
“Depending on the diagnostic and clinical capabilities of medical institutions, up to 50% of primary tumors may remain undiscovered for patients with this type of cancer,” said Andrew Birkeland, assistant professor in the Department of Otolaryngology-Head and Neck Surgery and the UC Davis Comprehensive Cancer Center and coauthor of the study. “Missing the primary tumors might put patients at risk of cancer spread and death.”

What is squamous cell carcinoma of unknown primary in the head and neck?
Carcinoma is a cancer that forms in epithelial tissues lining internal organs. Head and neck squamous cell carcinoma of unknown primary origin, also known as occult primary, is a clinical scenario when metastatic carcinoma is identified in the neck’s lymph nodes, but the primary tumor location is not identified by standard imaging or clinical exam methods.
Around 2600 new cases of occult primary cancer are identified each year in the U.S. They represent roughly 3%–5% of all new cases of head and neck carcinoma.
This type of cancer has no identified primary site. This means the original site where the cancer started is unknown, even after exhaustive clinical, radiographic and surgical evaluation. In most cases, especially those related to the human papillomavirus (HPV), the primary site is suspected to be in the palatine tonsils and the lingual tonsils of the base of tongue. These cancers are less likely to be associated with tobacco and alcohol abuse.
Integrating imaging technology into transoral robotic surgeries
Transoral robotic surgical platforms (TORS), such as the da Vinci® Surgical System, allow for minimally invasive surgeries to detect and remove tumors from hard-to-reach areas in the head and neck. To improve decision-making during surgeries and enhance the detection of elusive tumors, new diagnostic technologies compatible with TORS are needed.
“If surgeons can identify and visualize metabolic changes in tissue during the operation, they can precisely remove cancerous tissues and improve the patient’s survival,” Birkeland said.
What is FLIm and how does it work?
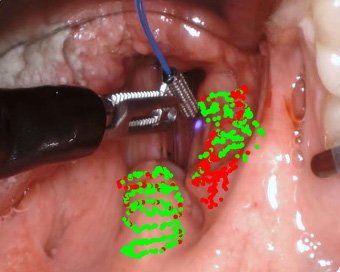
FLIm was developed at the University of California, Davis. The technology allows for the objective visual detection of tumors using the tissue’s intrinsic fluorescence properties. The surgeon scans the tissues for fluorescent changes related to alterations in tissue metabolism, a factor strongly linked to cancerous tumors. The FLIm device captures and analyzes the intrinsic light emitted by the tissues and provides visual and quantitative data of the autofluorescence light.
The technology has showed benefits in the diagnosis and surgical guidance in brain and breast cancer surgeries and potential in identifying heart disease.
This UC Davis homegrown technology might become the next standard of care, adopted widely in cancer surgeries.” —Laura Marcu
Findings
The team integrated FLIm into a transoral robotic system to acquire optical data on the oropharyngeal tissues of patients with head and neck carcinoma of unknown primary origin. These tissues are part of the throat at the back of the mouth, including the soft palate, the base of the tongue and the tonsils. The combined robotic-imaging power captured and analyzed tissue autofluorescence to differentiate tissue types.
The team first used a dataset of 55 patients with known primary tumors to train a machine learning classifier and develop a model that can accurately identify the presence and location of occult cancer using FLIm tissue autofluorescence.
Then, they looked at HPV-related cancers of unknown primary origin. They tested the accuracy of the model in six patients with occult primary head and neck cancer.
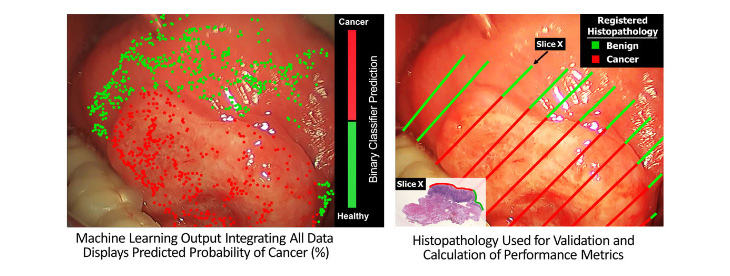
Among the six patients, HPV-related occult primary was surgically identified in three patients, whereas three patients ultimately had no identifiable primary site in the oropharynx. The FLIm model correctly detected the primary cancer site in all three patients and predicted benign oropharyngeal tissue for the remaining three. The mean sensitivity was 95% and specificity 89%.

“A key benefit of our FLIm technique is that it can highlight tumor infiltration in real-time during surgery,” said Laura Marcu, UC Davis professor of biomedical engineering and a pioneer of the FLIm technology. Marcu is the co-lead author on the study. “This UC Davis homegrown technology might become the next standard of care, adopted widely in cancer surgeries.”
This project was supported by the National Institutes of Health (R01 CA187427). This is an academic-industry partnership grant between UC Davis and Intuitive Surgical, Inc.
Coauthors on this study include Brent Weyers, Mark Marsden, Athena Tam, Julien Bec, Roberto Frusciante, Dorina Gui, Arnaud F. Bewley, Marianne Abouyared, and Donald Gregory Farwell.
Related stories:
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.