New genetic clues about melanoma revealed through powerful imaging
Researchers use molecular imaging to uncover the genetic factors that drive this aggressive skin cancer
New research from UC Davis Health maps the potential causes of the deadliest skin cancer down to the cellular level.
The study led by Maija Kiuru, professor of clinical dermatology and pathology, appears in the latest issue of Science Advances. By using powerful imaging to look inside melanoma cells, a team of researchers was able to see the complex genetic factors that drive this aggressive disease.
About melanoma and its symptoms
Melanoma is a type of skin cancer. It starts in the cells responsible for creating pigment, known as melanin. Melanoma often begins as an unusual-looking mole or skin bump. Symptoms include a large mole diameter, darkening of a mole, or a mole with irregular borders.
If not caught early, melanoma can be deadly. According to the American Cancer Society, melanoma accounts for only about 1% of skin cancers; however, it causes the majority of skin cancer deaths.
Mapping the gene markers in melanoma
Melanoma has causes that are environmental, such as sunlight, as well as genetic. In the UC Davis Health study, researchers examined how genetic factors influence the cancer’s behavior.

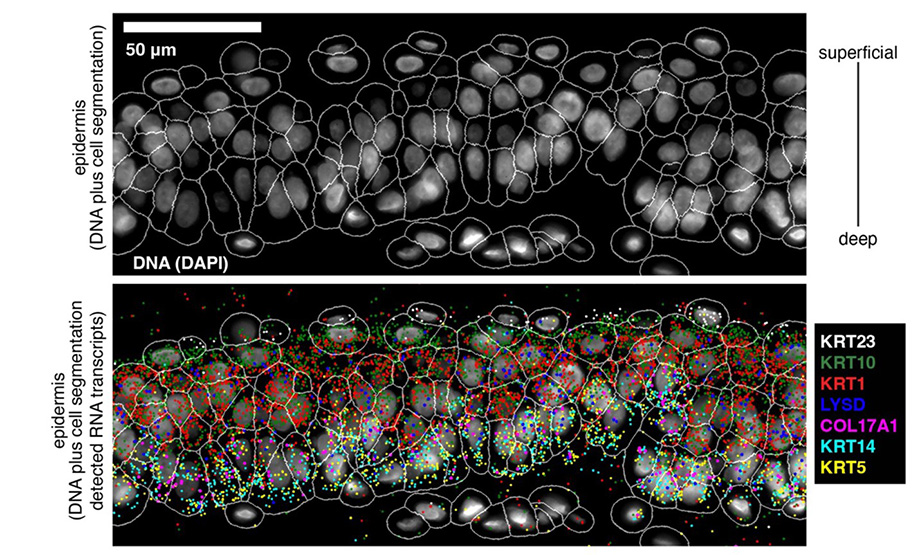
Researchers used a special technique called single-cell RNA-based spatial molecular imaging. The technique looks at the gene expression of thousands of genes at the level of individual cells without disturbing the tumor’s overall structure. The National Institutes of Health defines gene expression as “the process by which the information encoded in a gene is turned into a function.” For example, the insulin gene provides instructions for producing the hormone insulin to help regulate blood sugar.
With this powerful imaging, researchers were able to see patterns of gene activity in more than 200,000 cells in their native environment. They looked at cancerous and non-cancerous skin growths, ranging from harmless moles to aggressive, malignant melanomas. They identified gene patterns linked to cancer spread — patterns related to things like cell division, metabolism and cancer severity.
“This study shows how the spatial gene expression analysis at a single-cell level provides valuable clues about gene regulation in deadly cancers,” said Kiuru. “Better insights into gene regulation in melanoma could bring us closer to identifying markers of aggressive tumors and personalized treatments improving patient survival."


The two genes that predict poorer melanoma outcomes

Researchers found two genes that stood out as red flags: CDK2 and FABP5. These genes were more active in metastatic, or spreading, melanomas. When these genes experienced increased activity, referred to as upregulation, it predicted a poorer outcome for patients.
“Research on genetic characteristics will mean better, more personalized therapies for melanoma patients,” said Kiuru. “In the meantime, patients can help prevent melanoma. They can limit sun exposure: wear protective clothing, use sunscreen and seek shade. They also can keep an eye on skin changes.”
Kiuru was joined in the study by a team of researchers including UC Davis Health faculty members Nick Love, John McPherson, Hidetoshi Mori, Alexander Borowsky and Emanual Maverakis. Their paper is titled, “Melanoma progression and prognostic models drawn from single-cell, spatial maps of benign and malignant tumors.” It is featured in the July 12 issue of Science Advances.