Cleft Care Services
A cleft lip is a gap in the lip; a cleft palate is a gap in the alveolus (bones of the upper jaw and/or upper gum) hard palate (the bony roof of the mouth) and/or the soft palate (the muscle portion of the palate). Clefts are a birth defect that can occur when the two sides of the lip and/or palate do not grow together during a baby’s development very early in pregnancy, typically between weeks 5-12. A child may be born with a cleft lip, a cleft palate, or both.
Babies’ lips and palates develop during the first three months of pregnancy. Typically, the left and right parts of the lip come together, or "fuse," creating a continuous lip. In a similar way, the left and right parts of the palate come together to create a normal palate. A front-to-back line along the roof of the mouth can usually be seen where the "fusion" occurred. A cleft causes no pain for your child, and it is not usually dangerous or a medical emergency.
Unilateral, complete cleft lip


Bilateral, incomplete cleft lip


Clefts are among the most common anomalies found in newborn babies. Annually in the U.S., over 6,800 newborns (or about one in 600 babies) are born with a cleft. Left sided clefts are more common than right; some clefts are bilateral, affecting both sides of the mouth. Around one-third of clefts involve the lip and alveolar ridge (upper gum). Two thirds of all clefts extend through the entire palate. Cleft lip and palate occurs about twice as often in boys as in girls, whereas cleft palate alone is slightly more common in girls.
There are multiple causes of clefting. Clefts can occur in isolation (non-syndromic) or as a part of a syndrome (syndromic). Most clefts of the lip and palate are isolated (non-syndromic) and inheritance is most often multifactorial, with genetic and non-genetic factors interacting to cause the cleft.
There are two types of inheritance:
- In single gene inheritance, a feature appears as a result of a single gene carried by one parent.
- In multifactorial inheritance, a feature appears as a result of a number of genetic and nongenetic factors.
Diagnosing a cleft prenatally: Your doctor may use ultrasound (also called a sonogram) to determine if your unborn baby has a cleft. In some cases, ultrasound can return pictures of cleft lip as early as the 20th week of pregnancy. It is more difficult to get clear pictures of baby’s palate, which means a cleft palate may not be identifiable on ultrasound. Once a prenatal diagnosis of a cleft is made, your doctor will determine if the cleft is your baby’s only concern. If no other anomalies are identified, the cleft would be called an isolated or non-syndromic cleft. If multiple anomalies are noted, then the cleft is called syndromic, meaning it is part of a syndrome. Additional information is often requested including:
- Family history of clefts
- Maternal health issues
- Associated abnormalities
- Chromosomal abnormalities
Of all babies with cleft lip and palate, 10% to 15% are diagnosed with a syndrome or chromosomal abnormalities. If tests report that the child’s chromosomes are normal, the risk for a syndrome drops to 8% to 10%.
Feedings should be a pleasant experience for both you and your baby. Together, you and your feeding team will determine what type of help your baby needs to help them grow.
Babies born with cleft lips are typically able to breast or bottle feed just like other infants. However, infants born with cleft palates are not able to create the suction needed to pull milk from a regular nipple. It is likely that they will require a special bottle to ensure adequate milk flow for growth and development.
In the beginning, your baby might sneeze milk or have the milk come out of the nose. This is a normal finding. The amount will become less as the baby gets used to feeding. Babies with clefts can get tired quickly since they use more energy to eat. It will be important to keep a feeding log for your baby until a growth curve is established.
Tips for feeding your baby:
- Keep your baby in an upright angle for feedings, usually greater than 45 degrees, as this will help with any reflux you baby may be having.
- Making sure that the bottle is always tilted and the nipple is filled with milk to help reduce gas.
- Watch for a rhythmic pattern of suck, swallow, and breathing.
- Milk may come back out of your baby’s nose during a feeding. If this happens, wipe the nose and mouth. Pause and allow your baby to recover and cough, if needed.
- Burp your baby every 15 minutes during the feeding and again after feeding. Painful gas can occur if babies are not burped often, as babies with cleft palates swallow lots of air when they bottle feed. Wet burps are normal.
- Limit feeding sessions to 20-30 minutes to allow your baby to conserve energy and avoid losing calories while they eat.
- Hold your baby upright for 30 minutes after feeding to reduce to chance of spit ups.
- Stick to a feeding schedule. Missed feedings can lead to weight loss.
- Keep track of your baby’s weight gain; your baby should be back to their birth weight by two weeks of age, then gaining approximately 1 ounce a day (Paul, Schaefer, Miller et al., 2016).
Breastfeeding
The goal of breastfeeding is for your baby to gain weight and enjoy feeding. A few babies with clefts can get all of their food by nursing. Most can nurse a bit, but also need extra bottle feeding. Your baby’s success depends on the type of cleft and your milk supply.
- Babies with a cleft palate typically cannot get adequate nutrition to grow at the breast because they cannot create suction. However, you can put the baby to breast for bonding and to maintain your milk supply. Your baby can be fed expressed breast milk in a bottle.
- For babies with cleft lips, we advise putting your baby to breast several times and supplementing with pumped breastmilk or formula as needed. This helps to ensure your baby gets enough food in the beginning.
- Even if your baby is not nursing at the breast, breastmilk is still the best feeding choice for babies with clefts. Pumping is important, even from the very beginning.
- Your lactation consultant can help you set a pumping schedule that matches your baby’s needs. She can also teach you about milk storage.
- Accept help from family and friends to free your time to pump and rest.
- Spend “skin-to-skin” time with your baby to help support your milk supply.
Choosing a Nipple
Depending on the size and type of your baby’s cleft, he may need a special bottle or nipple to feed. There is no “perfect” nipple. The best nipple is the one that works best for your baby.
Some commonly used nipples include:
Drinking from a cup
- Babies with a cleft are usually able to use a cup around the same time as other infants, typically around 8-9 months of age.
- It is important to try out different cups, as your baby might show preference on one over another.
- It is helpful to establish cup drinking prior to palate repair surgery, as it is not recommended to immediately return to bottle feeding following the surgery.
- Children should be drinking exclusively from a cup by 1 year of age.
Tips for feeding solid food
You should be able to begin feeding your baby pureed foods with a spoon around the same time as other infants with the guidance of your pediatrician. Only introduce one new food a week when offering food so that you can watch for allergic reactions.
- 4-6 months: cereals (rice, oatmeal) and pureed baby foods
- 9-10 months: For beginning table foods, such as small pieces of soft well cooked vegetables (diced carrots, peas), soft breads and pasta, and small pieces of soft fruits (avocado, banana).

Cleft treatment and repair will start early in your child’s life to ensure both good health and normal development. Cleft lip and palate surgeries are done in stages and are planned based on your child’s facial growth. Cleft surgery is performed under general anesthesia and takes about two or three hours. Typically your baby will remain in the hospital 1-2 nights. The surgeon and the nursing team will instruct you on how to care for your child’s lip at home after surgery.
Pre-surgical Preparation


Lip Taping
Before your child’s surgical repair of the cleft lip you may be asked to use specialized tape to bring the edges of the cleft closer together. This may improve the overall appearance of the lip repair.
- Tegaderm (or DuoDerm) is placed on the skin to protect the skin from the adhesive on the Steri-Strips. Change the Tegaderm when it gets loose, about 4-5 days. Changing too frequently can be irritating to the skin.
- Change the Steri-Strips once a day or when they become soiled or loose.
The Nasal Alveolar Molding Appliance (NAM) is a way to treat cleft lip and palate. The NAM mold brings your baby’s lip and gum together by helping to move and reshape the cleft area as your baby grows.
- Nasal means that it fits up into the nose.
- Alveolar means that it fits around the gums.
- Molding means the gum line will be shaped with a small denture-like plastic appliance.
The device is usually fitted when a baby is about 2 weeks old and is worn 24 hours a day until the first surgery, usually around 4-6 months of age.
The mold is held in the mouth by surgical skin tape. The tape will also help guide the growth of your baby’s face. Each week, the orthodontist will reshape the mold, and will help to make your baby’s cleft smaller and reshape the nose.
Types of Surgery
Primary cleft lip repair: the surgeon makes incisions on either side of the cleft to create flaps of tissue and muscle which are sewn together to restore function, align muscle and lengthen the lip through advanced plastic surgery techniques.
Ear tube placement: recommended when your child has chronic fluid in the middle ear causing a conductive hearing loss of about 25-30dB. The ear tube is placed in the tympanic membrane (ear drum) and allows fluid to discharge out of the middle ear, air into the space to improve hearing and regulate air pressure of the ear.
Primary cleft palate repair: the surgeon mobilizes the palatal shelves, repositions the muscle and closes the hard and soft palate to recreate and restore function to the palate. The stitches are generally along the midline of the palate.
Velopharyngeal insufficiency (VPI) surgeries: approximately 20% of children with a cleft palate will need secondary palate surgery. The goal of VPI surgery to improve the structure and therefore the potential function of velopharyngeal closure for balanced speech resonance.
- Furlow palatoplasty: realign the muscles of the palate to lengthen and thicken the soft palate.
- Sphincter Pharyngoplasty: muscle is taken from the sides, rotated and sewn in to the back wall of the pharynx to narrow the velopharyngeal port. During speech the soft palate closes the centralized round opening to provide adequate pressure in the oral cavity for balanced speech resonance.
- Pharyngeal Flap: a passive, soft tissue bridge of tissue is created from the back of the pharynx and connected to the soft palate. During speech the lateral wall of the pharynx close against the bridge of tissue to allow adequate pressure in the oral cavity for balanced speech resonance.
Alveolar Bone Graft: to insert bone, typically from the hip, into the alveolar cleft to fill in the gumline and to provide adequate bone for the eruption of adult teeth.
Maxillary and Mandibular Distraction Osteogenesis: surgical procedure that lengthens the upper and/or lower jaw to get it in better alignment for dental occlusion.
Rhinoplasty: Construct adequate cartilage in the framework of the nose to provide good nose tip symmetry, height and definition.
The first three to five years of a child’s life are the most important years for speech and language development. Your cleft team speech-language pathologist will assess, and support your child to optimize their speech and language acquisition.
Cleft lip with or without a cleft of the alveolus (gumline) has impact on speech production. Your child may have distorted speech sounds produced behind the top front teeth (e.g., /s/ and /z/), at around 4 years of age. Your child will be assessed by your cleft team speech-language pathologist at 2 years of age.
Cleft Palate: Speech is one of the most common concerns of cleft palate repair. Somewhere between 50-75% of children with a cleft palate will require speech therapy during childhood and 20-30% of these children will need a second palate surgery to improve their speech and resonance (Sell, 2001).
Evaluations occur during the cooing and babbling sounds stage. Early babbling sounds are indicators of later speech and language skills. The soft palate is needed to provide adequate pressure in the mouth for all the consonant sounds except “m,n.” Parents and caregivers are encouraged to elicit nasal and low-pressure sounds made at the front of the mouth, such as “m, n, w, y, l, h,” as well as non-speech sounds (e.g. motorboats, lip smacks, tongue smacks, etc), to assist with sound production. Babies who produce more sounds before their initial cleft palate repair have better speech and language outcomes.
Children with cleft palate tend to develop speech and language a bit later than other children. A speech-language pathologist needs to regularly evaluate your child’s speech sound production in order to make appropriate and necessary recommendations. Your child’s first evaluation should be scheduled at about 8 months of age with follow up visits every 6 months for the next few years. These appointments will be coordinated with their surgeon and/or audiology visits as much as possible. And if speech therapy is found to be necessary, a speech-language pathologist can assist you with finding local resources.
Children with cleft palate can develop speech sounds in their throat to compensate for the oral pressure they cannot make in their mouth. These throat sounds can make it very difficult for others to understand what they are trying to say and can be very difficult to unlearn. It is important to work with your child and their speech-language pathologist to prevent and/or correct speech habits, so that your child can be understood by all potential listeners.
How to help your child in infancy through preschool years: You and your family can have a huge impact on your child’s speech and language. Helping your child to develop age-appropriate speech and language can lead them to develop successful communication skills for the rest of their life. It is important to remember that you and your family provide communication models for your child. In other words, your child will copy what you do or say. To help your child, you and your family can incorporate a few things into your daily routine. These things are listed below;
- Speak clearly and pronounce words well.
- Repeat words and phrases that your child says.
- Use short sentences (2-4 words) when talking to your young child.
- Avoid baby talk as much as possible (e.g. using fake or mispronounced words).
- Avoid making and encouraging growling, squealing or other throat-like sounds (e.g. dinosaur or monster sounds).
- Use the phrase “oh no” instead of “uh-oh” because it contains a glottal stop/throat sound.
- Name and talk during everyday activities such as walks, meals, bath time. (e.g. “First we are going to get your hair wet, then we use the shampoo.” “I see your eyes, nose and toes”).
- If your child appears interested in something, name and describe the object to them.
- Read books with your child every day - even five minutes a day can be helpful.
Speech and Language Development: During the preschool years, the team speech-language pathologist will be evaluating your child’s language and speech sounds. If your child’s speech and/or language are delayed, then the team speech-language pathologist will give you ideas of how you can encourage development and assist you with finding a local speech-language pathologist to help your child.
Resonance: Once your child is producing phrases with consonant sounds, their resonance will be evaluated. Hypernasality can occur when too much sound passes through the nose during speech. In contrast, speech may be hyponasal if sounds cannot pass into the nose when they should. This can sound similar to when you have nasal congestion with a cold or allergies. If it is hypernasal, a nasopharyngoscopy procedure will be considered when the team feels your child is behaviorally ready. This is a scheduled appointment with the team speech-language pathologist and your surgeon. Following some spray to numb and open the nasal passages, a spaghetti-sized camera will be placed in your child’s nose to look at the palate function while your child speaks sentences of their best speech. The procedure lasts from 2-4 minutes. During that appointment, findings and a treatment plan will be discussed with you and appropriate follow up will be scheduled.
Your child will have regular hearing tests with a pediatric audiologist as part of their care with the cleft and craniofacial panel. Good hearing is important for speech and language to develop normally as well as for overall brain development and advancement of social skills. Because children with cleft lip and palate can be at risk for ear and hearing problems, hearing and the health of the ears will be monitored regularly through childhood.
Infants with cleft palate have more difficulty with the function of the eustachian tube, which connects the middle ear space with the back of the throat. The eustachian tube is normally closed, however, it momentarily opens during chewing yawning or swallowing. This allows air pressure to equalize in the middle ear space and normal fluid to drain from the middle ear. If the eustachian tube does not open properly, fluid can collect behind the eardrum causing temporary hearing loss that fluctuates from mild to moderate. For some children, hearing loss is the only symptom but other children can develop acute ear infections with ear pain, fever, and irritability.
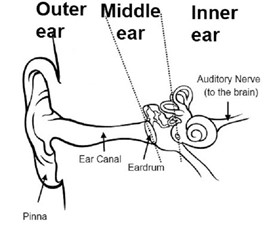
Middle ear fluid is more formally called otitis media with effusion and nearly all infants with unrepaired cleft palate will experience OME during their first year of life (Ponduri et al., 2009). Hearing loss due to chronic OME is usually managed medically and placement of tympanostomy tubes or “ear tubes” are often recommended. Ear tube placement can be scheduled at the same time as any other surgery that your child may have. The ENT surgeon will make a small hole in the eardrum and suction the fluid from the middle ear space. A tiny tube is then placed in the incision to keep the hole open. This will allow the middle ear to remain air-filled and prevent fluid build-up. Most of the time the tubes come out on their own and the eardrum hole heals naturally. Sometimes children have hearing loss that is not resolved by placement of ear tubes but may be the result of other problems with the ears. Your audiologist and ENT physician may recommend hearing aids for hearing loss that is expected to be longstanding or permanent.
Hearing and the function of the ears can be assessed at any age using a variety of tests. It is likely that your baby had a newborn hearing screening in their birth hospital. It is important to understand that a screening only identifies the need for further testing. Passing a hearing screening does not rule out mild hearing loss. The objective of audiologic testing is to determine whether there is any degree of hearing impairment that is affecting your child's access to spoken language and to help determine the cause. Hearing loss can vary in degree and there are different types of hearing loss depending on what part of the ear is affected. What follows is a description of some of the more common audiologic tests. None of these tests are painful. Hearing loss, if untreated, may result in difficulties in speech, social interactions, and academic performance. If a hearing loss is identified, the audiologist may recommend amplification.
Auditory Brainstem Response (ABR): For very young infants under the age of 6 months, ABR is the best method to estimate hearing levels. Electrodes are placed on the forehead and behind the ears while sounds are played through soft insert earphones. The test measures electrical waves generated by the hearing nerve and the brainstem. Your child needs to sleep for this test and it takes approximately one to two hours.
Tympanometry: This test measures whether the eardrum is moving normally. A soft rubber tip is placed in your child’s ear and a quiet humming noise is present during a gentle air pressure sweep. Tympanometry is used to assess whether middle ear fluid is present, whether pressure in the middle ear is equalized, and is also useful for determining whether ear tubes are working or not.
Otoacoustic Emissions: This test looks for a tiny response from the hair cells of the inner ear that create energy in response to incoming sounds. A soft tip is placed in the ear and the child hears various tones, while a sensitive microphone measures tiny sounds generated by the ear itself. When the response is present we know that hearing is likely normal or near normal but this test does not give us hearing threshold levels.
Behavioral audiometry: Any hearing test where a response from the patient is required is considered a behavioral test. Sounds used to assess hearing include tones of various pitches that are important for hearing and understanding speech, as well as speech itself. Older children and adults can raise a hand or push a button in response to sound but we use specialized techniques to measure hearing behaviorally with children as young as six months. The techniques used depend on the age and development of the child and include:
Visual Reinforcement Audiometry (age 6 months to 2 or 3 years of age): The baby or toddler is trained to respond to a sound presented through loudspeakers or headphones by pairing the head turn response with a lighted video display to reward the response.
Conditioned Play Audiometry (age 2 to 5 years): The young child is engaged in a “listening game” were they may be asked to place a toy in a bucket or a peg in a board when they hear beeping tones through headphones.
Just like any other child, a child with a cleft will require good dental care throughout life. It is common for children with a cleft to have a variety of dental issues which will require specialized treatment from dentists and orthodontists.
Dental care: With proper cleaning and nutrition, children with a cleft are able to have healthy teeth. Once teeth erupt from the gums between 6-9 months of age, they should be wiped with a damp cloth after each feeding, this prevents milk being left on teeth which can cause cavities. For this reason, it is very important that your child not go to sleep with a bottle in their mouth.
It is recommended that children see a pediatric dentist for a check-up around their first birthday. Regular follow-ups every 6 months are recommended throughout their life. Cleaning should be done at least twice a day for two minutes, as soon as the first teeth erupt. Parental supervision and participation is important until your child is 8 years old.
It can be challenging to get children in the routine of brushing their teeth. Below are a few fun ideas to get your kids excited about keeping their teeth clean and healthy.
How To Get Kids Excited About Oral Health
- Start a routine and stick with it: It can be tempting to skip brushing your child’s teeth (or your own teeth) after a long day, or perhaps even when you are running late in the morning. However, the more consistent you are, the more likely they are to stick with the routine.
- Make it fun with the Mouth Monsters: Tooth D.K., Ginger Bite-Us and Tartar the Terrible present a fun way to talk to your kids about tooth decay and why brushing is important to keep the Mouth Monsters away. Download the Mouth Monster mini posters that you can hang up on the bathroom mirror as a reminder, and check out “Denty Land,” a fun and interactive game full of great tips for parents and kids.
- Let little ones show off: Parents should participate in brushing until age 7 or 8 to make sure kids are doing a thorough job. In the early years, take advantage of little ones’ growing sense of independence and let them show YOU their tooth-brushing skills before you help out.
- Tooth-brushing tunes: Two minutes can seem like an eternity to a child. To help pass the time and make it fun, play one of their favorite songs on your phone, sing a song or even make up a song for two minutes.
- Practice makes perfect: If your child has a favorite doll or stuffed animal, you could have them pretend to brush their doll’s teeth, too – good oral health is important for everyone!
Orthodontics: Children born with cleft lip and/or palate are often have missing or misshapen teeth. This is most common when the cleft extends through the gums. The majority of children with a cleft require multiple phases of orthodontic treatment, which span through childhood and adolescence.
The goal of orthodontics:
- to improve appearance of teeth
- to align top and bottom teeth for chewing
- to make teeth easier to brush
Treatment may include traditional braces, as well as specialized orthopedic appliances such as expanders and head gear in preparation for surgery. It is recommended that children see a local orthodontist by age seven. Orthodontic treatment depends on the surgical procedure needed and is important to the success of both the surgery and health of the teeth. Orthodontic care is often coordinated with the cleft and craniofacial team orthodontists to get the best results.





