Utilizing Education and Post-Discharge Support to Enhance Outcomes for Chronic Obstructive Pulmonary Disease Patients
According to the U.S. Centers for Disease Control and Prevention, chronic obstructive pulmonary disorder (COPD) was the third leading cause of death among U.S. citizens in 2011—with more than 15 million Americans diagnosed with the condition. Additionally, COPD has been included as one of the key conditions listed by the Centers for Medicare and Medicaid Services in its Hospital Readmission Reduction Act—by which hospitals and health systems can incur financial penalties if target benchmarks in care are not met. Due to this high rate of mortality and prominence in quality measures, many hospitals and health systems have made better managing patients with COPD an organizational priority.
The UC Davis Medical Center—a 619-bed academic medical center in Sacramento—exemplifies this drive to improve outcomes for COPD patients with its implementation of the Reversible Obstructive Airway Disease (ROAD) program. In order to learn more about the ROAD program’s efforts to support COPD patients throughout the discharge and post-hospital care process, The Academy spoke with Dr. Samuel Louie, Professor, Director of the UC Davis Asthma Network, and Director of the ROAD Center.
Enduring Education
As is the case when managing many chronic conditions, patient education plays an important role in both reducing readmissions and improving outcomes and overall quality of life. To that end, the ROAD program at UC Davis focuses its efforts on providing patients with comprehensive education about how to self-manage their condition and reduce the likelihood of exacerbations—the usual cause of both readmission and mortality.
“Severe COPD exacerbations can be more deadly than a heart attack and many patients have no idea about the danger or how to get help,” Dr. Louie says. “Increasing the danger is that almost all exacerbations begin at home or in the patient’s daily life, so our goal was to put patient safety first by providing them with education.”
The patient education service provided by the ROAD program differs from many other organizations’ programs because it is conducted while the patient is still in the inpatient setting. As soon as patients are admitted to the hospital, they are flagged for enrollment in the ROAD program through provider word-of-mouth or through the use of a screening tool embedded in UC Davis’s electronic health record (EHR)—which looks for elements such as smoking history or use of respiratory medications.
Following their enrollment in the program, patients are provided with four educational sessions by the ROAD program team members which each last approximately 20 minutes. Beginning on their first day of admission, patients are educated on foundational information about COPD, the medications they will
be prescribed and how to use them, how to recognize impending exacerbations, and what their post discharge care plan will be. By educating patients in this one-on-one, progressive manner, the information is presented in an individualized fashion that has a more lasting impact than the more common classroom approaches to post-discharge patient education utilized by many organizations.
“To see the difference between one-on-one education and classroom-based education, all you have to do is visit a classroom in any of our esteemed universities here in the U.S. and look around at all the people falling asleep,” Dr. Louie explains. “By going to the patient’s bedside and personally engaging with them to provide education in a manner that is palatable and approachable, we are providing patients with enduring value and education that they can be prepared to leave the hospital with.”
Specialist Staffing
Beyond the implementation of engaging patient education practices, the utilization of the best staff can often drive significant improvements in quality. Again unlike its counterparts at other organizations, UC
Davis employs respiratory therapists for the ROAD program rather than the more commonly utilized nurse practitioners. Each of these respiratory therapists is certified as a COPD case manager, allowing them to provide both inpatient education services and to coordinate patients’ post-discharge care.
“We employed respiratory therapists because they’re cheaper than nurse practitioners and are better suited to the task in many ways,” Dr. Louie says. “They are a group of expert healthcare professionals with every bit as much dedication and empathy—which is what these patients really need.”
Even after the inpatient episode of care, the ROAD program’s respiratory therapists continue to support patients as needed. Following discharge, patients are provided with a phone number giving them direct access to members of the ROAD team, which they can call with any questions or concerns between 7:00 a.m. and 7:00 p.m.. Additionally, all patients are referred to pulmonary rehabilitation services to assist them in developing further self-management techniques.
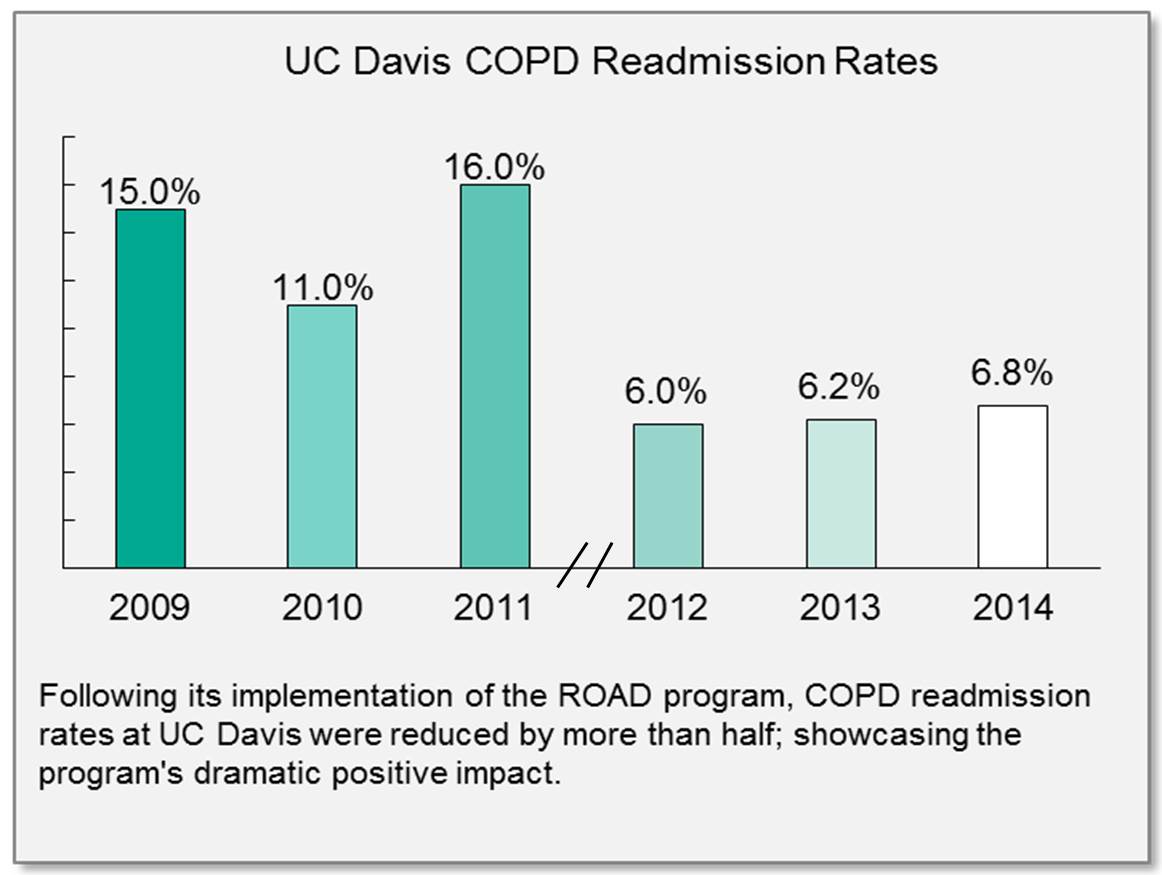
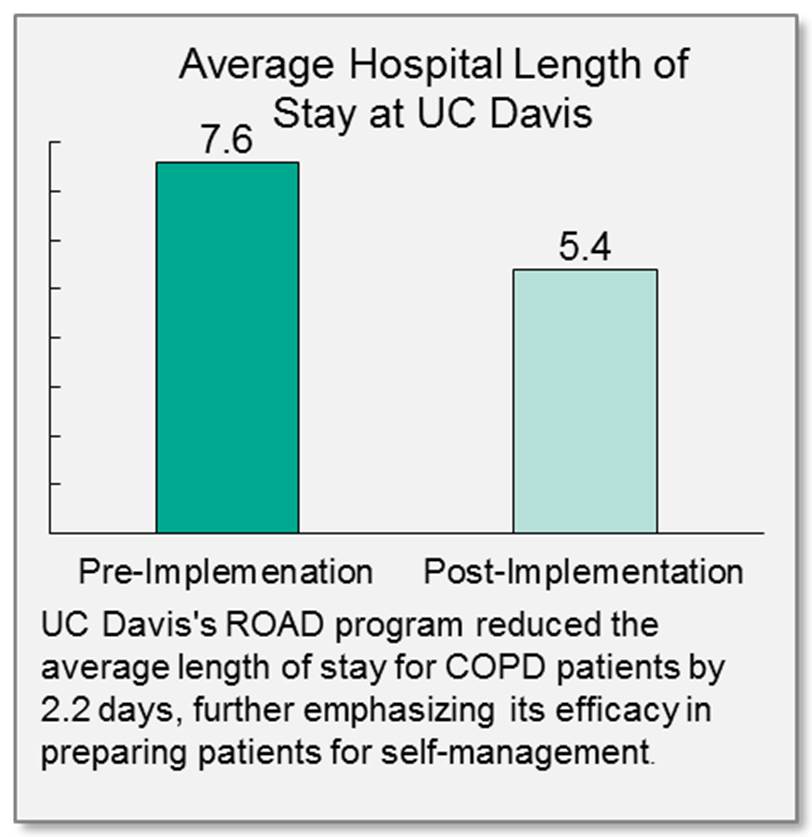
As a result of this dedicated post-discharge support and comprehensive inpatient education, UC Davis’s ROAD program has resulted in significant reductions in both readmission ates and length of stay for patients with COPD. Prior to the program’s implementation, UC Davis’s COPD patient readmission rate fluctuated between 15% in 2009, 11% in 2010, and 16% in 2011. These readmission rates were cut by more than half after the ROAD program’s implementation to 6% in 2012, 6.2% in 2013, and 6.8% in 2014. Furthermore, the average length of stay for COPD patients was reduced from 7.6 days to 5.4 days—despite the provision of more involved inpatient education services.
For leaders looking to improve protocols for managing COPD patients, the practices of the ROAD program at the University of California, Davis can serve as a helpful example. By employing a team of specialists dedicated to providing individualized educational services and post-discharge support, the ROAD program is not only benefitting hospital operations, it is improving its patients’ quality of life.
“We emphasized the concept of reversible when naming our program because we want our patients to know that there is hope,” Dr. Louie concludes. “Not only is lung function partially reversible, but hospital readmissions are reversible, exacerbation frequency is reversible, and quality of life is reversible.”
Krystal Craddock, RRT, NPS, CCM
Program Coordinator
916-734-7113
