The Lupus Clinical Care Program
Addressing healthcare disparity and equitable access to lupus care.

The Lupus Clinical Care Program
At UC Davis Health, patients are at the center of everything we do. The mission of the Lupus Clinical Care Program starts with putting patients first by:
- Addressing healthcare disparities and provide equitable access to care.
- Improving patient outcomes through timely, collaborative patient centered care.
- Enhancing lupus awareness among the community, patients and their families.
- Training and educating our future rheumatologists and healthcare workforce.
- Bridging patient access to innovative therapeutics including novel clinical trials.
- Creating a better understanding of the onset, progression and outcomes in lupus.
Why Lupus Care?
Lupus Foundation of America (LFA) estimates that around 1.5 million Americans suffer from lupus. It affects women significantly more and disproportionately affects certain population subgroups especially ethnic and racial minorities with greater prevalence and potentially more severe disease course. With its significant impact not only on patients but also their caregivers, families and society at large, there is growing urgency to better understand its onset and progression, identify enhanced treatments and deliver these equitably to our patients to improve outcomes. A comprehensive multi-specialty approach is vital for delivery of care and improving outcomes in lupus. It is also important that the care approach is not limited simply to “management” of active inflammation but rather addressing it in a holistic patient centered care approach.
Systemic Lupus Erythematosus (SLE) is a multiorgan disease that can affect any organ system in our body and is associated with risk of organ damage and significant morbidity. Its incidence and prevalence have seen a dramatic rise over the past few decades in the United States, in part due to better identification of the disease, care and treatment options available today. Mortality associated with SLE has improved over the last few decades but when compared to all-cause mortality rates, continues to remain higher, especially in population subgroups including females, and across racial minorities.
We don’t know exactly what causes the onset and progression of SLE. Multiple genetic factors have been implicated to play a role and a strong family history is a concern for potential development of SLE. In addition, environmental factors are thought to have a strong influence in a susceptible individual developing the disease and its progression. Some of the most important implicated factors include exposure to ultraviolet radiation especially the sun, certain infectious agents especially viruses, and smoking and tobacco exposure.
Early, accurate diagnosis of SLE is essential in controlling the disease and improving long term outcomes through appropriate evidence-based interventions. The diagnosis of SLE is based on clinical assessment by a trained provider and includes thorough review of contributing history and examination findings, with additional laboratory evidence and imaging where required. There are several “classification criteria” available to aid in grouping SLE patients with common factors but are not diagnostic by themselves alone.
Since SLE has the potential for organ damage and associated with significant morbidity and mortality, early detection and management of the disease is key to long term improved outcomes. The European League Against Rheumatism (EULAR) strongly recommends consideration for multidisciplinary individualized care under a shared decision-making model. It also recommends regular disease assessment at patients’ visits and including both pharmacologic and non-pharmacologic options for optimal treatment and outcomes.
Medications that alter or suppress the immune system are important for disease control in SLE and include options like hydroxychloroquine, mycophenolate mofetil, methotrexate, rituximab, leflunomide, belimumab, cyclophosphamide and azathioprine. Corticosteroids (including prednisone, prednisolone and methylprednisolone) are usually intended for short term use for disease control and sometimes used in very low maintenance doses. Based on our improved understanding of the disease over the years, in addition to medications that suppress the immune system attention to bone health by improved weight bearing exercises, optimal calcium and vitamin D intake and other interventions are important. Also noted is the importance of a healthy active lifestyle, nutritious balanced diet, and avoidance of ultraviolet/sun and smoking exposures.
Heart disease is the leading cause of death among patients with SLE, especially women in the younger age groups and racial minorities. Early evaluation and mitigation of cardiovascular risk factors in SLE is very important.
You can also find additional therapeutic information through the American College of Rheumatology.
While control of disease activity and inflammation is the primary objective in management, SLE is frequently associated with chronic comorbidities including other potential autoimmune disorders, as well as chronic fatigue, chronic pain and depression. Chronic concerns such as persistent ongoing pain, fatigue symptoms, depression and sleep disorders generally do not respond to suppression of the immune system and require focused attention and management by the care team, including their primary care provider. It may also need additional specialists to help understand and mitigate the impact of these conditions on the patients’ lives.

Patient Focused Providers
Gaurav Gulati is a board-certified rheumatologist offering care for adult patients with autoimmune rheumatologic conditions including lupus, rheumatoid arthritis, inflammatory myopathies, and others. He believes in treating an "individual" and not merely a disease condition, and appreciating patients' goals of care and preferences through collective decision making.
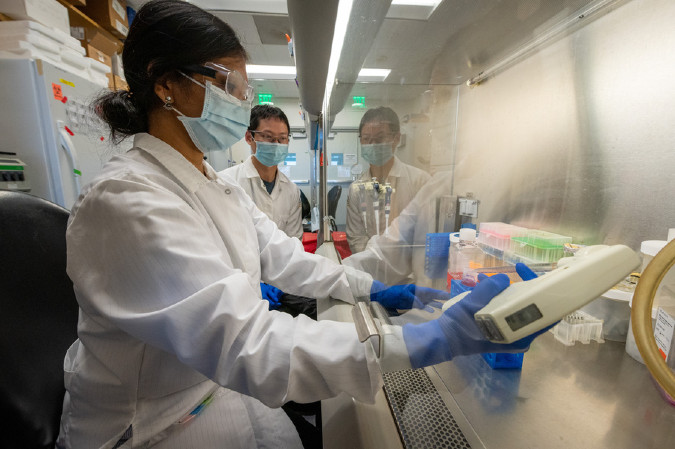
Science Based Solutions For Our Patients
Our researchers are constantly working on emerging treatment options to help combat Lupus. Our program emphasizes the integration of physician educators in research to develop superior practitioners, directly translating into excellent patient care.