Gastroschisis: A newborn bowel condition that requires specialty care
Gastroschisis is a complex and costly birth condition that affects babies’ bowels. Cases have doubled in the United States over the last two decades.
We talked with Geoanna M. Bautista, an assistant professor of pediatrics in the Division of Neonatology at UC Davis Health Children’s Hospital, to learn about gastroschisis. She also shared the best practices for caring for newborns with the condition.
Bautista’s research focuses on gastrointestinal diseases that affect newborns. She is especially interested in premature births and birth defects that impact normal gut development, including gastroschisis. She has spearheaded the establishment of the UC Davis Baby Intestines Group (B.I.G.). It is a collaborative initiative among neonatology, gastroenterology and surgery to improve the outcomes, growth and longitudinal care of newborns at high risk for intestinal failure, such as babies with gastroschisis.
What is gastroschisis?
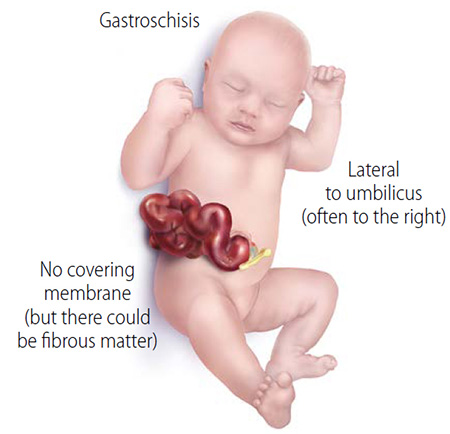
Gastroschisis develops during pregnancy. It is an abdominal wall defect that prevents the gut from growing properly and causes problems in the gut's muscles and nerves (dysmotility). The developing baby has an opening in the abdomen through which their intestines spill out into the surrounding amniotic fluid. With time, the unprotected intestine becomes irritated, causing it to swell, shorten and become inflamed.
Gastroschisis is unique in that it disproportionately affects younger mothers. It also appears to be associated with environmental factors, although the underlying causes and development are still poorly understood.
When is gastroschisis diagnosed?
Gastroschisis is often diagnosed during the anatomy scan (ultrasound) performed around 16 weeks gestation. In some cases, it is not found until after the baby is born, usually due to limited or no prenatal care.
If diagnosed prenatally, parents typically get referred to a hospital with a level IV Neonatal Intensive Care Unit (NICU), such as UC Davis Health Children’s Hospital, that has access to specialist surgeons.
Does gastroschisis come in different severity levels?
Gastroschisis severity varies widely. Most babies born with the condition have “simple” gastroschisis. This means no other intestinal complications developed in utero. “Complex” gastroschisis, on the other hand, is linked to conditions such as intestinal atresia (blockage), perforation (hole in the bowel’s wall), ischemia (not getting enough blood or oxygen), and necrosis (death of tissues). These conditions may have developed later in gestation and are often not discovered until after the baby is born.
Gastroschisis is unique in that it disproportionately affects younger mothers.”—Geoanna Bautista, neonatologist at UC Davis Health Children's Hospital
What happens when babies with gastroschisis are born?
Babies with gastroschisis can often be delivered vaginally, which surprises most parents since the baby’s intestines are literally outside their body. At the delivery, it is very important that the bowel is handled with the utmost care as any compression can cause injury. The bowel outside the body can also lead to dehydration and electrolyte changes. It needs to remain moist at all times. The baby will also need a lot of fluids.
How is gastroschisis treated?
Surgical correction of the original defect occurs shortly after birth. The babies are brought to the NICU where surgeons evaluate the defect size, the amount of bowel, and if any other organs, such as the liver, have also managed to herniate out.
Babies get one of two repairs: A primary repair, which means the surgeons put the intestines back into the abdominal cavity directly after birth or a staged reduction, which means the intestines are slowly placed back into the abdomen little by little to avoid.
After the repair surgery, there is often a long monitoring period until the baby has adequate bowel function and motility before we slowly introduce milk.
What are some health complications linked to gastroschisis?
We have come a long way in optimizing neonatal management and postnatal repair of the original defect. Yet, these babies often struggle with delayed gut motility and function due to the damage that happened in utero.
About 20% of babies with gastroschisis develop necrotizing enterocolitis (NEC), a disease that causes inflammation and death of tissues in the intestine. Thus, some babies may need to have part of their intestines removed due to atresia (obstruction) or from the development of NEC. This may lead to short bowel syndrome, intestinal failure and life-long challenges.
Babies that don’t require additional surgeries or resections can still have problems with dysmotility and absorption of nutrients. This can further impact growth and development.
What is the best way to care for a baby born with gastroschisis?
Typically, the hardest part for parents is seeing their babies “repaired” but continuing to wait for their bowels to function normally. Then feeding is slowly initiated and advanced Most babies can get through this period in the NICU without additional complications. Once they tolerate full feedings and grow appropriately — which can often take several weeks to months — they can be treated like any other newborn and taken home.
Typically, the hardest part for parents is seeing their babies “repaired” but continuing to wait for their bowels to function normally.”—Geoanna Bautista, neonatologist at UC Davis Health Children's Hospital
The babies still need careful monitoring even if they do not require additional surgeries. Some can have poor growth and have nonspecific GI symptoms, like constipation.
Unfortunately, babies with gastroschisis may also develop complications and require multiple surgeries. Those babies are more likely to have lost a significant amount of bowel. They may go home needing IV nutrition and continued follow-up with our intestinal rehabilitation program. I always tell parents that every baby is different.
What could be driving inflammation in babies with gastroschisis?
We still don’t know what is driving this inflammation. Our team believes a signaling pathway may be the missing link in understanding gastroschisis-related complications.
This is truly an exciting time in science. We now have better tools and a greater understanding of some of the mechanisms driving these impairments in other similar disease processes. We have also moved towards a more collaborative team science approach. This means our efforts translate into true clinical benefit for these babies.
Are there interventions that can help developing babies with gastroschisis in the womb?
There are currently no in-utero interventions available for gastroschisis. There is growing interest in developing fetal interventions that focus on earlier targets to hopefully prevent the ongoing damage that clearly affects normal gut development.
Thanks to Drs. Diana Farmer and Shinjiro Hirose who established the Fetal Care and Treatment Center (FCTC) and the Center for Surgical Bioengineering (CSB) co-led by professor Aijun Wang, UC Davis has truly become a hub for pioneering fetal interventions that result in amazing outcomes. With this kind of environment and resources, I anticipate that my current collaboration with Dr. Hirose will lead to new efforts and success at intervening in these developing babies before they are born.
Bautista recently received awards from the Hartwell Foundation, the Children’s Miracle Network and the Clinical and Translational Science Center KL2 award.
Related stories:
Necrotizing Enterocolitis - Dorian's Story at UC Davis Children's Hospital




