New research explains mechanisms behind psoriatic arthritis
Findings could lead to more effective therapies against autoimmune skin disease
A study by UC Davis Health showed how inflammatory proteins called cytokines take the brakes off synovial cell growth in joints, leading to the abnormal tissue accumulation that’s associated with psoriatic arthritis.
The research led by rheumatologist Siba Raychaudhuri presented at the American College of Rheumatology Annual Meeting in November, revealed some of the molecular mechanisms that underpin this disease and highlighted how new, targeted therapies could help alleviate it.
Psoriasis and psoriatic arthritis are two sides of the same autoimmune coin. In both cases, immune cells — mostly T-cells — mistakenly target healthy tissue, causing inflammation and cell overgrowth of keratinocytes in skin (psoriasis) and synovial cells in joints (psoriatic arthritis).
“Synovial cells line joints and produce synovial fluid to lubricate them. We wanted to understand whether cytokines are inducing synovial cell proliferation and playing a direct role in pannus formation,” Raychaudhuri said.
Over time, psoriatic disease destroys the joints.
“We can see the damage as it affects joint membranes, synovial membranes and bones, which ultimately leads to arthritis. As you can imagine, this causes patients tremendous pain and loss of function,” Raychaudhuri said.
Rampant synovial cell growth
The study focused on how inflammatory molecules drive pannus formation. The key is an enzyme pathway in T-cells called JAK/STAT.
In healthy cells, the enzyme JAK (Janus Kinase) activates STAT proteins to turn on genes associated with the inflammatory immune response and other traits. However, when this pathway goes awry, it can lead to a wide variety of autoimmune and inflammatory conditions, including lupus, rheumatoid arthritis and psoriatic disease.
In psoriatic arthritis, T-cells migrate to joint tissue, releasing inflammatory cytokines. Scientists have long known that these cytokines activate the JAK/STAT pathway, leading to massive inflammation. However, this study adds another chapter to the story, showing JAK/STAT activation also drives synovial cell hyperproliferation and pannus formation.
This study provides new insights into the role JAK plays in pannus formation, which can be so debilitating for patients with psoriatic arthritis.”—Siba Raychaudhuri
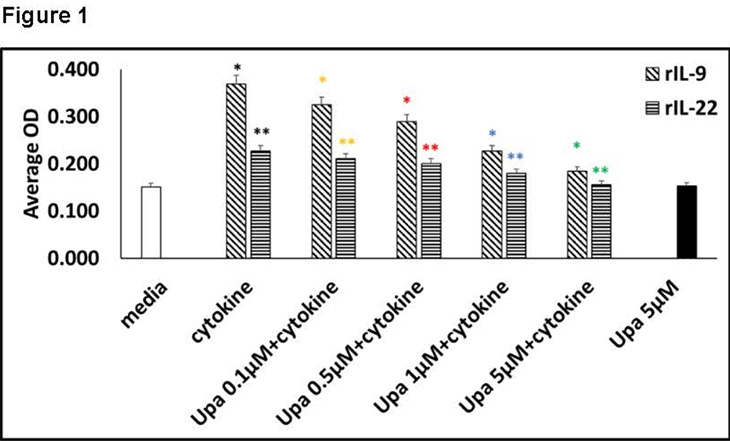
“JAK/STAT is influenced by several cytokines in psoriatic arthritis, including IL9 and IL22, ultimately leading to an increase in the? number of synovial cells,” Raychaudhuri explained. “However, when we inhibit JAK, we can see that proliferation is reduced. These findings show that JAK plays a key role regulating synovial cell proliferation.”
From a clinical standpoint, this research showed that inhibiting JAK reduced abnormal tissue formation and the associated joint damage, revealing how JAK-inhibiting drugs could be used to moderate psoriatic arthritis.
“This study provides new insights into the role JAK plays in pannus formation, which can be so debilitating for patients with psoriatic arthritis,” Raychaudhuri said. “Medications can be developed to directly target the pannus. While there are existing FDA-approved JAK inhibitors, there is definitely scope to improve them for better efficacy against rheumatoid arthritis, psoriasis and psoriatic arthritis.”
The coauthors on this study are Christine Abria and Smriti K Raychaudhuri of the Sacramento VA Medical Center.
Similar Stories: