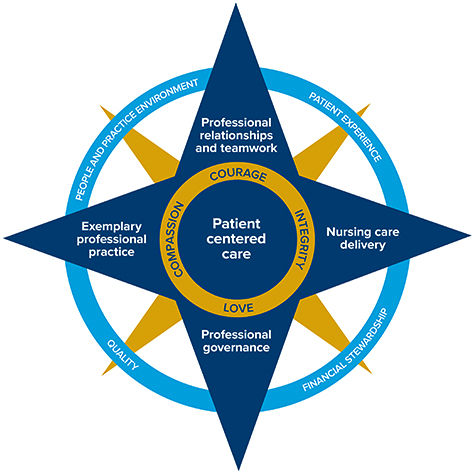
Professional Practice Model
What is a professional practice model (PPM)?
A professional practice model describes how registered nurses practice, collaborate, communicate, and develop professionally to provide the highest-quality care for those served by the organization.
Why do we need a PPM?
The UC Davis Medical Center PPM defines the foundation and components of professional nursing practice. . The PPM aligns and integrates nursing practice with the mission, vision, values and philosophy of nursing. The framework of our PPM guides the nursing strategic plan, identifying clear goals and expectations for all professional RNs. Through the PPM we achieve optimal outcomes.
Values
Extraordinary Love, Compassion, Courage, Integrity, in every situation!
Mission
Provide science-based, technologically precise, compassionately delivered patient care.
Vision
The highest quality of patient care provided through the advancement of nursing practice.
Philosophy
WE, The Nurses of UCDMC Believe that our mission is to provide science-based, technologically precise, compassionately delivered nursing care; Define nursing as a scientific discipline that takes a holistic approach to the diagnosis and treatment of potential and actual responses to illness with a goal of lessening the effects of illness, promoting comfort and healing, and assisting patients to achieve an optimal level of self-care; Practice in a dynamic university medical center that promotes ongoing learning for all health professionals; Strengthen our practice through a commitment to innovation and nursing research; Accept professional accountability to patients, families and the community; Recognize the uniqueness of each person, and respect, protect and advocate for the individual's right to self-determination, self-expression, confidentiality and dignity; Believe that we best serve through collaboration with other health care professionals who join with us in treating and advocating for those who need our nursing care; Believe that the relationships we build have an inherent capacity to promote health, healing, and wholeness; Commit ourselves to support, acknowledge and nurture one another, thereby creating an environment of mutual respect and caring.
Core Values
We employ a code of ethics upon which we base our daily practice. Ethics is a foundation to our professional practice. Our beliefs stem from several sources; American Nurses Association (ANA)Code of Ethics, ANA Scopes and Standards of Practice, our organizational values and our personal values.
Primary Nursing
Primary Nursing is a relationship-based model which includes therapeutic presence, autonomy, evidence-based practice, and collaboration. Nursing presence is a relationship between the nurse and the patient in which the nurse approaches the patient in a holistic way recognizing each patient as a unique individual. Primary Nursing is based around the elements of responsibility, accountability and authority.
Resources
We have a variety of resources available to provide optimal patient care. As part of a leading university, nurses have access to the latest research and leading edge technology. We have opportunities to consult with experts in a variety of health-related fields including: chaplaincy, child life, food and nutrition services, occupational therapy, pharmacy, physical therapy, medicine, respiratory therapy, social work and speech therapy.
Nurses also have autonomy to provide holistic approaches such as: essential oils, music therapy, pet therapy, and the HUSH (Help Us Support Healing) initiative.
Relationship-Based Culture
We believe everything in health care will work better when relationships are healthy since relationships permeate every aspect of health care. All the technical aspects of health care occur in the context of human relationships, which means all of the technical tasks underlying the provision of care work better when we tend to relationships. Healthy relationships are formed when nurses consistently attune to one another, wonder with and about one another, follow the cues provided by one another, and hold one another with respect and dignity. We advance our relationship-based culture through the application of these relational and therapeutic practices to all relationships at all levels and in all disciplines.
Relational and Therapeutic Practices
- Attuning – The practice of being present in the moment and tuning in to an individual or situation.
- Wondering – The practice of being genuinely interested in a person. It requires an open-hearted curiosity about what can be learned about this unique individual, while intentionally suspending assumptions and judgement.
- Following – The practice of listening to and focusing on what an individual is teaching us about what matters most to her or him and allowing that information to guide our interactions. It requires consciously suspending our own agenda.
- Holding – The practice of intentionally creating a safe haven to protect the safety and dignity of an individual.
Relationship-Based Care
The Relationship-Based Care model (Koloroutis, 2004) is the philosophy, way of being, and operational blueprint which shapes our caring behaviors. The model’s sievenprinciples guide the transformation of infrastructure, processes, systems, and practices to support care givers in all disciplines in creating therapeutic relationships with patients and families.
Relationship-Based Care identifies three key relationships for the provision of humane and compassionate healthcare. These relationships are the nurse’s relationship with self, team members, and patients and families. We use this order, not to signal priority, but to acknowledge certain relationships dependency on others. Healthy, trusting relationships depend on how individuals relate to themselves. Healthy h patient and family relationships depend on the relationships individuals have both with themselves and with their teams.
Principles of Relationship-Based Care
Healing Culture – Our healing culture holds all people with respect and dignity. All are supported in reaching their full potential and are valued for their contribution to the health and healing of patients. Therapeutic relationships and a calming physical environment are core components of our healing culture.
Loving Leadership – Our leadership is one of service. Our servant leaders share power, puts the needs of others first, and help people develop and perform as competently as possible. A Loving leadership is key ingredient for leaders aspiring to advance a more positive healing culture. Inspired leaders who love what they do and the people with whom they do it, inspire others to greatness. Loving leadership is marked by deep affection and caring for those with whom we work and lead. Love in leadership means truly caring about each person, celebrating successes, as well as having empathy in times of struggle. It includes releasing judgment and forgiving past difficulties. It means being fully present in our interactions.
Teamwork – We embrace a shared purpose and work together with trust and mutual respect across all disciplines and departments. Nurses collaborate with all disciplines of the health care team to achieve best patient outcomes. This requires consistent and coordinated care of a patient through a unified plan of care, and information sharing amongst health care team members.
Interprofessional Practice – Our clinical professionals are respected and valued for their unique expertise and full scope of practice. Clinical practice is grounded in research, professional standards, and ethics. “Clinical competence” is the combination of both technical and relational competences. We accept that different perspectives of people in multiple disciplines are essential to effective collaboration and optimal patient care and outcomes. We allow for all practitioners to bring their best wisdom to the interdisciplinary group. We follow formula of Responsibility + Authority + Accountability to facilitate greater personal ownership and alignment with and among teams.
Care Delivery – We facilitate the ability of each caregiver to know the patient as a person and to provide care based on what is most important to the patient and family. We hold the following three rules:
- Hold the patient and family at the center of our care
- Make the best way the easiest way
- Support all relationships
We believe that designing the delivery system using these simple rules actively promotes the conditions for care that is safe, effective, patient-centered, timely, efficient and equitable.
System design – We are continuously improving our structures, processes and relationships to bring quality, safety, effectiveness and efficiency to patient care and the work environment. We are improving our systems to allow clinicians to focus on what is most important, safe and efficient. We approach any change with rigorous methodology and humble and curious attitude. Our just culture framework and the four relational practices of attunement, wondering, following and holding are in place to support a system that is both relationally and technically proficient.
Evidence – We have outcomes that show evidence of success, such as Magnet®recognition and the Beacon and Prism awards that are sources of inspiration. Our achievements of actualizing our vision and mission are evident in our nursing practice. We express clear expectations, are recognized and recognize others for the value each brings to the work of the organization, and celebrate successes that continually build commitment and unity.
Healthy Work Environment
We believe that a healthy work environment is an essential element in creating the context for engagement in the professional practice of nursing. A healthy work environment is actualized through alignment with the six standards for establishing and sustaining healthy work environments identified by American Association of Critical Care Nurses:
- Model and educate techniques for skilled communication.
- Work to collaborate with each other and other disciplines by identifying and engaging stakeholders and seeking feedback for our nursing practice.
- Be effective decision makers as evidenced by our policies, councils, and committee involvement.
- Continuously evaluate the appropriateness of our staffing practices through patient outcomes, patient experience, and nurse engagement.
- Recognize our contribution to the organization through established programs to promote nursing practice.
- Embrace our practice with the responsibilities and privileges it brings.
Measuring Nurse Engagement
Nurse engagement is measured by Press Ganey through the employee engagement survey. UC Davis Medical Center nurses show high engagement and autonomy scores and feel strongly that they have opportunities to influence nursing practice and have the freedom to act in the best interest of their patients. They value the ability to effectively communicate and collaborate with interprofessional teams. They feel valued and believe there are opportunities to learn and further develop professionally throughout their careers. We are engaged in action planning to improve their work environment.
Recognition
Recognition of the nursing profession is both formal and informal. Nurses are recognized many ways for their clinical expertise, leadership, compassion and caring. Formal recognition may include: serving as a preceptor or committee member, gaining support to present work at a national/international conference or internal presentation, and receiving the prestigious DAISY award. Informal recognition occurs daily and comes from knowing one has done a good job, from patients and their families, and from peers and leaders.
Coaching and Mentoring
Experienced nurses mentor and support new graduate nurses as they progress through the Vizient/American Association of Colleges and Nursing (AACN) Nurse Residency Program. The coaching provided by preceptors, clinical facilitators, and mentors helps new nurses as they acquire the knowledge, skills, and confidence to provide safe quality care.
In addition, as professional nurses we acknowledge our collective role in sharing our knowledge and expertise with our peers through both informal and formal mentoring opportunities. As we move through our careers, we maintain our commitment to providing positive role models for others and obtain new mentors for ourselves as needed.
The Rising Nurse Leader (RNL) program supports and guides our next generation of nurse leaders. Each participant is paired with a nurse mentor who exemplifies nursing leadership and can provide knowledge, support and guidance in navigating the complex and demanding roles in clinical and managerial leadership. This mentorship inspires and gives confidence to the mentee while providing the mentor with a valued colleague.
Community Outreach
As community leaders, nurses are committed to improving the health of our local and international communities. RNs improve the health of the community through events such as blood pressure screening, health and safety fairs, and immunization clinics.
Professional Growth and Development
We believe in creating an environment that promotes professional learning, growth, and development. We view learning as a life-long process, which is essential to the professional growth and development of nurses who strive to deliver optimal patient care in a rapidly changing health care environment.
Professionalism
Professionalism informs the conduct, aims, and qualities that characterize the profession of nursing and an individual in the profession. It is determined by cognitive, attitudinal, and psychomotor attributes – how we comport ourselves with fellow nurses, interprofessional colleagues, patients and families. Attributes of professionalism in nursing at UC Davis Medical Center include knowledge, a spirit of inquiry, accountability, autonomy, advocacy, innovation and vision, collegiality and collaboration, and ethics and values. We offer a variety of processes and resources to enhance these attributes.
Our nurses support professional nursing practice through the peer review process, through which we examine and ensure adherence to the highest standards of our profession. This process supports many of the attributes of professionalism in nursing at UC Davis Medical Center. Individuals, institutions, and the nursing profession benefit from effective peer review. Participation in the peer review process stimulates professional growth and offers opportunities to set and achieve new goals for ourselves as professional nurses.
Advancing our Profession
UC Davis Medical Center nurses seek to advance our profession, taking up the charge of the Institute of Medicine (IOM) Future of Nursing Report to act as full partners in the transformation and improvement of health care. We are engaged in shaping the future members of our profession as we share clinical expertise at regional nursing schools on a variety of topics. Wecollaborate with peers and teach our nursing and interdisciplinary colleagues internationally. We provide fellowship opportunities to advanced practice providers seeking to learn from our team. We are engaged in our professional organizations as leaders, board members, and committee volunteers, and actively work to advance our profession.
Just Culture
We are committed to a just culture. We encourage the reporting of errors, lapses, near-misses, and adverse events. It is through this reporting and event analysis we learn what went wrong, or could have gone wrong, and how to prevent it from happening again. Our attention is on identifying and correcting system imperfections, supporting systems to help our staff learn from errors, near misses and prevent recurrences, while distinguishing human errors and system errors from unsafe, blameworthy actions.
Clinical Expertise
Nursing specialty certification obtained through professional nursing organizations is encouraged and supported through financial support and course offerings. We believe that nursing specialty certification contributes to better patient outcomes.
We place a high value on professional development in order to provide optimal care topatients and to achieve personal and professional satisfaction.
Evidence-Based Practice
Nurses integrate clinical expertise, patient values and preferences, and the best research evidence to guide nursing care to achieve optimal outcomes. We use the IOWA Model of Evidence-Based Practice is used to promote excellence in health care.
Research
We seek answers to clinical questions when evidence is not available to inform practice. Nurse-initiated research is an important part of clinical inquiry at UC Davis Medical Center. We collaborate as leaders and as co-investigators in research that generates scientific discovery and insight into the human experience. The UC Davis Health Center for Nursing Science promotes the development of nursing science and its implementation in practice.
Optimal Outcomes
We provide individualized, holistic patient and family centered care. Optimal outcomes are achieved through high quality care, the nursing delivery care model (primary nursing), skilled communication, leadership and teamwork. Wecollaborate on performance improvement initiatives, implement evidence-based practice, adhere to clinical practice standards and participate in research to achieve optimal outcomes.
Leadership
Nurses at UC Davis Medical Center are transformational leaders at all levels. They are respected for their expertise and structures are in place to support engagement in the professional practice of nursing. Nurse leaders use their clinical expertise to advocate for professional practice and to advocate for human and fiscal resources. Teamwork and collaboration help achieve optimal outcomes.
Professional Governance
Professional governance is a structure that empowers professional clinical nurses to contribute collaboratively as decision makers regarding the nursing practice environment. This includes standards of practice, policies and procedures, resource utilization and stewardship, evidence-based practice and research, and quality and performance improvement. The system-wide councils exist to support the Unit-Based Practice Councils. The purpose of the system-wide governance councils is to coordinate the activities to outcomes in the areas of nursing, evidence-based practice and research, education, relationship-based care, nursing excellence, technology, and nursing quality.


