Physician assistant student pinpoints undiagnosed heart issue
Trusting his gut and his training prompted Nick Woods to speak up after hearing unusual sound in his stethoscope
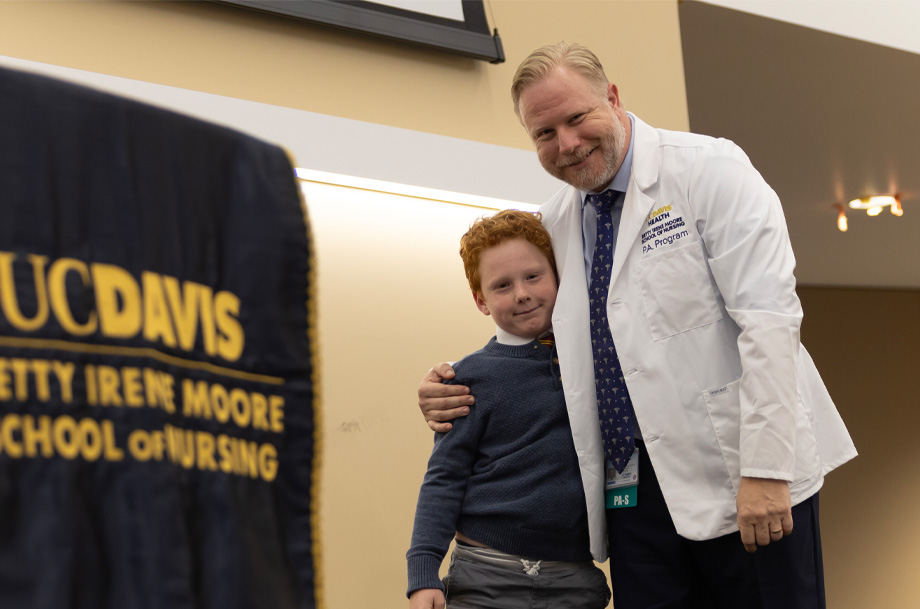
Nick Woods had one more exam to take before completing his first quarter in graduate school. As a physician assistant student at the Betty Irene Moore School of Nursing at UC Davis, the 40-year-old needed to demonstrate his classroom knowledge and hands-on skills.
He was performing a head-to-toe physical assessment on an actor playing the role of patient. Woods entered the simulation room — set up to mimic a primary care clinic — and began going through his checklist. After taking his patient’s vital signs, he placed his stethoscope on the patient’s chest to check his heart rate. That’s when he heard a sound that stopped him in his tracks.
“It was something I’d never heard before,” Woods recalled. “It sounded like a bump, whoosh.”
Could it be a heart abnormality? Woods wondered. But how could he be sure? He debated whether to say something to his “patient.”
Role playing that mimics reality
Mitch Darnell is what is known as a standardized patient. Standardized patients are actors who follow a script and role-play the ailments a typical patient might see a primary care provider for. Darnell has played the part for eight years at UC Davis Health for hundreds of students in the School of Nursing’s physician assistant (P.A.) program, like Woods, and the UC Davis School of Medicine.
“I watch the students’ body language as they enter. I’m in character as a patient, being vulnerable, waiting to see how they respond to me as the patient, see if they respect this patient,” Darnell explained. “Nick is the kind of guy who came in with confidence and exhibits strong respect and consideration for this patient.”
Confidence that masked nervousness, perhaps. Woods knew some basics about caring for patients from his three years as an emergency medical technician before graduate school. But in the primary care clinical simulation suite, his desire to do well on his skills test — even though students had not yet experienced in-depth cardiology instruction— kept him focused and quiet.

Bump, whoosh.
“The sound was so obvious that I was arguing with myself that he had to already know about it, right? Woods recalled himself thinking out loud. “Surely, his doctor or another student has told him. I didn’t want to derail the exam, but I also didn’t realize how severe a murmur could be. I just wasn’t confident in what I was hearing.”
Darnell, meanwhile, had no idea that Woods’ stethoscope had picked up an unusual beat.
“He played his cards to his chest,” Darnell said. “I didn’t see any reaction. I had no clue.”
Woods headed home. But on the 30-mile drive back to Vacaville, the bump, whoosh played over and over in his head. That nagging feeling prompted him to pull off the road and email his professor, Phil Emond, who was still in the simulation suite. Darnell was there too, so Emond took a listen.
“Discoveries like this happen usually from second-year students who relate feedback on how they were able to figure out a diagnosis while in a clinical rotation as a result of their preparation, practice and training,” said Emond, a P.A. with 40 years of clinical experience. “It shows an incredible amount of maturity and confidence on Nick’s part as well as a strong desire to help the patient.”
It also underscored how UC Davis models for students how to interact with patients.
“They were graceful and told me not to be overly stressed, but to not wait to call my primary care doctor,” Darnell said. “I left there with a great understanding of what to do.”
A week and a half later, Darnell’s physician confirmed he had a leaking atrial valve. When a valve is leaky, it fails to close properly, resulting in the backward flow of some blood into the heart. If not addressed, this condition could lead to heart failure. For Darnell, the condition could be further complicated by his sleep apnea and epilepsy. Darnell now requires periodic check-ins, for the rest of his life.
The encounter between Woods and Darnell last year serves as a learning opportunity for future students.
“It’s one thing to listen to a normal heartbeat, but how do you know if you didn’t pick up on something,” Darnell wondered. “It’s great that students have me to hear something that’s not normal. It’s a beautiful teaching moment that people can have in real life.”
Life and art meet
The goal of UC Davis’ standardized patient program is to provide high-quality learning and assessment opportunities for health care students. The actors portray different types of patients who engage in realistic, improvised, simulated scenarios with students. These encounters test not only the students’ clinical competency, but also their judgement and communication skills.
“The value of the program lies in the students' ability to learn, practice, grow and test their clinical and physical exam skills in a safe space with people who have been specifically trained to work with them in ways that prioritize their learning,” explained Melissa Thew, program director at the time of Woods’ discovery. “The scope of the ways that students and standardized patients work together is far and wide, and it can be very fulfilling and purposeful work for the actors.”
Especially when life and art meet, as was the case with Woods and Darnell. The takeaway for both is immeasurable.
Trust your training and trust your instincts. It’s proof that what we’re being taught works in the real world.—Nick Woods, first-year physician assistant student
“Trust your training and trust your instincts. It’s proof that what we’re being taught works in the real world,” Woods said.
“We’re moving into a world where A.I. is taking over. This program is brilliant because subliminally people learn to talk to people about their health. The human interaction, the little things they pick up and read at a glance, tone of your voice is vital for humanity,” Darnell added.
Woods has moved on to new curriculum, cardiology included. But his discovery serves as a lesson to his classmates and future students that their 27 months in school sets the stage for their future in the P.A. profession.
“It reminds all of us — faculty, staff and students — to never lose focus on how important and effective a program like this is in developing competent and compassionate health care providers to help address disparities,” Emond said. “Our students never cease to amaze me.”






