Stem Cell Transplant Program
Our program offers various options with success rates that meet or exceed national averages in Northern California.
Stem Cell Transplant Program
Stem Cell Transplant Services
UC Davis Comprehensive Cancer Center offers comprehensive stem cell transplant services. Our expert team of doctors, nurses, and specialists guides patients and donors through the process.
We provide state-of-the-art facilities for stem cell collection, storage, and safe transplantation within a dedicated Bone Marrow Transplant Unit.


Advanced Transplant Care at Cancer Center
The Stem Cell Transplant Program at the UC Davis Comprehensive Cancer Center has a groundbreaking history. We performed the region’s first bone marrow transplant in 1998.
We continue to offer extensive transplant options with success rates that match or surpass national averages.
Care and Collaboration
As an National Marrow Donor Program (NMDP) Transplant Center, we provide access to a vast network of stem cell donors and cord blood. We're also committed to participating in vital national clinical trials, ensuring our patients benefit from cutting-edge research.
Our priority is compassionate and personalized care for patients, donors and their families. This collaborative approach is focused on achieving the best possible outcomes for everyone involved.
Hematopoietic stem cells are immature cells that develop into:
- red blood cells – also called erythrocytes, which carry oxygen to organs and tissues
- white blood cells – also called leukocytes, which fight infections
- platelets, which help the blood to clot
All these cells play a crucial role in the healthy functioning of our bodies. Most stem cells are found in bone marrow, which is the spongy tissue inside large bones. Some cells also are found in the blood stream. Blood from the umbilical cord also contains hematopoietic stem cells. Cells from any of these sources can be used in transplants.
Stem cell transplantation is a treatment for a wide range of diseases including blood cancers such as leukemia, lymphoma and myeloma. It can cure some diseases and put others into remission.
Depending on the stem cell source, the procedure may be called a bone marrow transplant, a peripheral blood stem cell transplant, or a cord blood transplant.
In stem cell transplantation, patients are given intensive doses of chemotherapy and/or radiation therapy to kill cancer cells. At the same time, this treatment destroys the normal cells in bone marrow. To re-establish production of cells in bone marrow, patients must receive an infusion of healthy stem cells previously collected from a patient or stem cell donor.
There are three transplant types, which differ depending on the stem cell donor source. Each type involves a different procedure and carries different side effects and risks. The type of transplant recommended depends on several factors, including the patient’s type of disease, age and overall health, and donor availability.
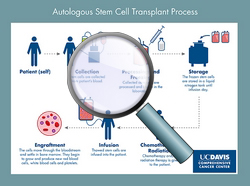
Autologous transplant
“Auto” means self. The patient donates his/her own stem cells prior to a high dose of chemotherapy or radiation.
Click here to enlarge illustration
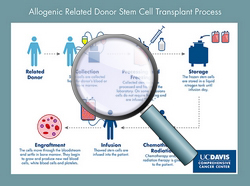
Allogeneic: related donor transplant
“Allo” means “other”. Stem cells are donated by another person, the donor. This type of donor is a genetically matched family member (usually a brother or a sister).
Click here to enlarge illustration

Allogeneic: unrelated-donor transplant
The person donating stem cells is not biologically related to the patient but genetically partially matches the patient. Unrelated donors may be found through the National Marrow Donor Program.
Before the transplant, chemotherapy or radiation or both are given. This pre-transplant treatment may be done in two ways:
Myeloablative (ablative, high intensity):
Myeloablative means marrow-destroying. During this treatment, a high dose of chemotherapy, radiation or both are given to destroy any cancer cells. This treatment also kills all remaining healthy marrow. Patients receive an infusion of new stem cells to rebuild the blood and immune system. In cases in which a patient's own stem cells are healthy enough, they are transplanted (autologous transplant); otherwise, transplanted cells come from a donor (allogenic transplant).
Non-myeloablative (reduced-intensity):
During the non–myeloablative treatment patients receive lower doses of chemotherapy and radiation, followed by an infusion of stem cells from a matched donor. This treatment eliminates some, but not all, of the patient’s bone marrow. It also reduces the number of cancer cells and suppresses the patient’s immune system to prevent the rejection of the transplanted cells. The reduced-intensity treatment allows older patients and patients with other health problems to have a transplant.
Stem cells used for transplants can come from three sources:
Peripheral (circulating) blood
Stem cells are collected from peripheral blood in a process called apheresis. The stem-cell donor blood circulates through a machine called a cell separator that removes the peripheral blood stem cells and returns the rest of the blood to the body. Because the concentration of stem cells in circulating blood is ordinarily very low, donors are given medications to stimulate the bone marrow to produce more stem cells. These cells are then released into the blood stream. The collection of stem cells from circulating blood is an outpatient procedure, and the donor (or patient) usually goes home the same day.
Peripheral stem cells are used most often in stem-cell transplantation for both autologous and allogeneic transplants.
Bone marrow
Bone marrow collection (also known as bone marrow harvest) is a surgical procedure that takes place in a hospital operating room. The collection is performed under general or spinal anesthesia. The stem cell donor does not feel significant pain or discomfort during the marrow collection. The bone marrow is removed with large needles from the flat pelvic bones. The donor may go home the same day or stay overnight in the hospital. Historically, this was how all stem cells were collected for transplantation, hence the common use of the term “bone marrow transplantation.”
Blood in the umbilical cord collected after birth
A newborn’s parents can donate umbilical cord blood to a public cord blood bank (where available) at no cost. Umbilical cord blood is rich in stem cells, and increasingly hospitals have the ability to collect these stem cells using special kits. The collection process does not pose any health risk to the infant and uses blood that would otherwise be thrown away. After the baby is born and the umbilical cord has been cut, blood is retrieved from the umbilical cord and placenta. The cord blood is then processed, frozen and stored until needed for a transplant patient.
Because cord blood cells are less immunologically mature than cells collected from adult donors, they can be used for transplantation even when the match between patient and donor is not perfect.
Apheresis services is staffed with experienced physicians and registered nurses trained in apheresis procedures and committed to providing the highest quality patient care.
Apheresis services provides clinical support to all UC Davis Medical Center programs including the stem cell, kidney and lung transplant recipients, utilizing state-of- the-art equipment to provide the following types of services:
- Peripheral blood stem cell collections, both autologous and allogeneic
- Therapeutic cell collections
- Therapeutic apheresis:
- Therapeutic plasma exchange
- Red blood cell exchange
- Photopheresis therapy to treat graft-versus-host disease and other indications
- White blood cell and platelet depletions
The department also serves as the only National Marrow Program (NMDP) apheresis center in the greater Sacramento area for the collection of donor peripheral blood stem cells and therapeutic cells. These cells are used in transplants for patients all over the world.
The cancer center’s apheresis services is registered by the U.S. Food and Drug Administration and licensed by the California Department of Public Health for producing biological products for treatment of humans. It also shares the Foundation for the Accreditation of Cellular Therapy (FACT) accreditation with the clinical section of the Stem Cell Transplant Program.
Our Hematopoietic Progenitor Cell Laboratory (HPCL) team has extensive experience in the field of cellular therapy and Good Tissue Practices including:
- Processing and freezing (cryopreservation) of stem cells derived from peripheral blood and bone marrow
- Plasma reduction and red-cell depletion of apheresis and bone marrow products when major or minor ABO incompatibilities between donor and patient exist
- Long-term storage in liquid nitrogen storage tanks and management of stem cells
- Thawing of cryopreserved stem cells for re-infusion
- Preparation of donor lymphocyte infusions
- Thawing and washing of cord blood
- Shipping frozen stem cells to other stem cell transplant centers
HPCL utilizes a continuous monitoring and alarm system for 24/7 control of stem cell storage.
HPCL collaborates with the Good Manufacturing Practices (GMP) Laboratory at the UC Davis Institute for Regenerative Cures and with other stem cell research groups. It also participates in innovative research projects leading to development of new treatments utilizing stem cells.
HPCL is accredited by the Foundation Accreditation for Cellular Therapy (FACT) and the College of American Pathologists. It is also registered by the U.S. Food and Drug Administration and licensed by the California Department of Public Health for producing biological products for treatment of humans. These accreditations and licenses indicate that the laboratory meets or exceeds the standards and regulations required for manufacturing of stem cell therapy products.
The Bone Marrow Transplant Unit (BMTU) has eight single isolation rooms with private bathrooms. Each room has an anteroom where family and staff wash their hands and put on a gown before entering the patient’s room.
The design of the BMTU includes a system that provides positive pressure airflow and a high efficiency particulate air (HEPA) filtration system to minimize presence of potentially infectious germs. Rooms are equipped with a cardiac monitoring system that allows staff to continually monitor patients during chemotherapy and stem cell infusion. Each room also has dedicated medical examining equipment to minimize the chance of transmitting infection to the patient. The BMTU also maintains a negative pressure room for patients with possible airborne infections.
Only authorized personnel and visitors are allowed in the inpatient BMTU.
Nursing care is provided by registered nurses trained and experienced in the management of stem cell transplant patients. Physicians are available 24/7.
UC Davis Medical Center, the facility where the Bone Marrow Transplant Unit is located, is accredited and certified by the Joint Commission. The certification is a symbol of quality for the healthcare organizations and reflects commitment to meeting certain performance standards.
Our Team
Medical Director of Transfusion Services
Associate Professor, Department of Pathology and Laboratory Medicine
- Specialties
- Pathology - Anatomic
- Pathology - Clinical
- Blood Banking/Transfusion Medicine
- Location(s)
- Phone: 800-2-UCDAVIS (800-282-3284)
- Phone: 916-734-2011
Distinguished Professor
- Specialties
- Hematology/Oncology
- Biological Chemistry
- Molecular Biology/Medicine
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Internal Medicine
- Cancer
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor (HSCP)
- Specialties
- Hematology/Oncology
- Cancer
- Oncology
- Breast Cancer
- Thyroid
- Breast
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Assistant Professor
Assistant Professor in Residence
- Specialties
- Cancer
- Molecular Biology/Medicine
- Hematology/Oncology
- Sarcoma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Director, Cancer Control/Cancer Disparities
- Specialties
- Cancer
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor
- Specialties
- Hematology/Oncology
Vice Chief, Hematology & Oncology
Director, Clinical Breast Cancer Program
Professor of Medicine
- Specialties
- Breast Cancer
- Hematology/Oncology
- Internal Medicine
- Breast
- Head and Neck
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Faculty Physician
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 800-362-5566
Professor of Medicine
- Specialties
- Breast Cancer
- Sarcoma
- Hematology/Oncology
- Internal Medicine
- Breast
- Melanoma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 916-734-5959
- Phone: 800-362-5566
Chief Medical Officer, International Society of Liquid Biopsy
Co-Director, Center for Experimental Therapeutics in Cancer
Senior Advisor to Director, UC Davis Comprehensive Cancer Center
Adjunct Clinical Professor, Translational and Clinical Research Program, University of Hawaii Cancer Center
Professor Emeritus
- Specialties
- Lung Disease
- Hematology/Oncology
- Internal Medicine
- Lung
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor of Medicine
- Specialties
- Adult Hemophilia
- Benign and Malignant Hematology
- Thrombosis
- Internal Medicine
- Hematology/Oncology
- Location(s)
- Phone: 800-482-3284
Assistant Professor, Division of Hematology and Oncology, Department of Internal Medicine
- Specialties
- Genitourinary Cancers
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor of Medicine
- Specialties
- Breast Cancer
- Cancer
- Oncology
- Hematology/Oncology
- Breast
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor of Medicine (HSCP)
- Specialties
- Geriatric Oncology
- Benign and Malignant Hematology
- Hematology/Oncology
- Leukemia
- Lymphoma
- Myeloma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor of Medicine
- Specialties
- Epidemiology
- Cancer Survivorship
- Hematology/Oncology
Medical Director, UC Davis Comprehensive Cancer Center’s Office of Clinical Research
Associate Professor of Medicine (Clin X)
- Specialties
- Oncology
- Gastrointestinal Cancers
- Hematology/Oncology
- Colorectal (Colon)
- Esophageal (Throat)
- Liver
- Pancreas
- Stomach
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Distinguished Professor
- Specialties
- Hematology/Oncology
- Biological Chemistry
- Molecular Biology/Medicine
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Director, UC Davis Comprehensive Cancer Center
Executive Associate Dean for Cancer Programs
Professor of Medicine
- Specialties
- Cancer
- Hematology/Oncology
- Adrenal Cortical
- Bladder
- Kidney
- Lung
- Prostate
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Physician Diplomate
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor, Department of Internal Medicine, Division of Hematology and Oncology
- Specialties
- Lung Disease
- Breast Disease
- Hematology/Oncology
- Breast
- Lung
- Location(s)
- Phone: 800-362-5566
Assistant Professor, Division of Hematology and Oncology
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor of Medicine and Chief Translational Officer
Associate Director for Translational Research, UC Davis Comprehensive Cancer Center
- Specialties
- Cancer
- Oncology
- Hematology/Oncology
- Prostate
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Internal Medicine
- Cancer
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor of Medicine (Reg)
Center Director, Stem Cell Program and Gene Therapy Center, Institute for Regenerative Cures, UC Davis
- Specialties
- Stem Cell Biology
- Research
- Bone Marrow Transplant
- Location(s)
- Phone: 916-703-9300
Associate Professor, Division of Hematology and Oncology
- Specialties
- Genitorurinary
- Hematology/Oncology
- Adrenal Cortical
- Bladder
- Kidney
- Prostate
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Director, Thoracic Oncology
Associate Professor of Medicine (Clin X)
- Specialties
- Cancer
- Lung Disease
- Head and Neck Cancer
- Hematology/Oncology
- Head and Neck
- Lung
- Parathyroid
- Thyroid
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Adjunct Professor
- Specialties
- Hematology/Oncology
- Breast
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor
- Specialties
- Bone Marrow Transplant
- Epidemiology
- Leukemia
- Lymphoma
- Myeloma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 800-362-5566
Assistant Professor of Clinical Medicine
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Physician Diplomate
- Specialties
- Hematology/Oncology
- Internal Medicine
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Assistant Professor
- Specialties
- Oncology
- Cancer
- Lung Disease
- Endocrinology
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Physician
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 800-2-UCDAVIS (800-282-3284)
- Phone: 916-734-2011
Professor
- Specialties
- Bone Marrow Transplant
- Leukemia
- Lymphoma
- Myeloma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Assistant Professor
- Specialties
- Oncology
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Chief, Division of Hematology and Oncology
Director/PI UC Davis Clinical and Translational Science Center
Associate Dean for Research
Professor of Medicine
- Specialties
- Hematology/Oncology
- Leukemia
- Lymphoma
- Myeloma
- Location(s)
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Hematology/Oncology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Assistant Professor
- Specialties
- Cancer
- Bone Marrow Transplant
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor
- Specialties
- Bone Marrow Transplant
- Internal Medicine
- Stem Cell Transplant
- Malignant Hematology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor of Medicine (Clin X)
- Specialties
- Leukemia
- Bone Marrow Transplant
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Professor of Medicine (Reg)
Center Director, Stem Cell Program and Gene Therapy Center, Institute for Regenerative Cures, UC Davis
- Specialties
- Stem Cell Biology
- Research
- Bone Marrow Transplant
- Location(s)
- Phone: 916-703-9300
Associate Professor
- Specialties
- Bone Marrow Transplant
- Epidemiology
- Leukemia
- Lymphoma
- Myeloma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor
- Specialties
- Internal Medicine
- Medical Oncology
- Bone Marrow Transplant
- Malignant Hematology
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner Supervisor
- Specialties
- Stem Cell Transplant
- Malignant Hematology
- Location(s)
- Phone: 800-362-5566
Professor
- Specialties
- Bone Marrow Transplant
- Leukemia
- Lymphoma
- Myeloma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Nurse Practitioner
- Specialties
- Bone Marrow Transplant
- Malignant Hematology
- Location(s)
- Phone: 800-362-5566
Apheresis Medical Director
Associate Professor
- Specialties
- Blood Banking/Transfusion Medicine
- Apheresis and Special Coagulation
- Location(s)
- Phone: 916-734-2525
Associate Professor
- Specialties
- Pediatric Hematology/Oncology
- Stem Cell Transplant
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566
Associate Professor
- Specialties
- Pediatrics
- Pediatric Hematology/Oncology
- Hematology/Oncology
- Sarcoma
- Location(s)
- Phone: 916-734-5959
- Phone: 800-362-5566























































