Epilepsy detectives: New unit helps doctors locate and diagnose seizures more effectively
Expanded monitoring unit specializes in guiding treatment for people whose epilepsy is not controlled by medication
The UC Davis Comprehensive Epilepsy Program has opened a new 11-bed epilepsy monitoring unit that specializes in diagnosing and guiding treatment for people whose seizures are not controlled by medication.
It is the largest such unit in inland Northern California that is accredited by the National Association of Epilepsy Centers as a level 4. This is the highest-level designation. It is only given to facilities equipped with the most sophisticated intensive neurodiagnostic monitoring technology and that perform the full array of treatments for epilepsy and other seizure disorders.
The new hospital unit was dedicated at a ribbon-cutting ceremony on Jan. 26.
David Lubarsky is the vice chancellor of human health sciences and CEO of UC Davis Health. At the ribbon-cutting, he celebrated this important milestone. “This epilepsy monitoring unit will make a difference in our patients’ lives in a way no other unit in the area can,” he said.

The science and experience of the epilepsy monitoring unit
One out of every 100 people experiences epilepsy. Two-thirds of these patients experience relief through medication alone, while the remaining one-third require treatments that may include surgery.
There are about 20,000 people in Northern California whose seizures are not controlled by medication.
UC Davis offers the latest surgical treatment options, including minimally invasive procedures such as laser ablation, robotic-assisted surgery, and neuromodulation. To operate effectively and safely, doctors must determine both the specific kind of seizure a patient experiences and where it originates in the brain.
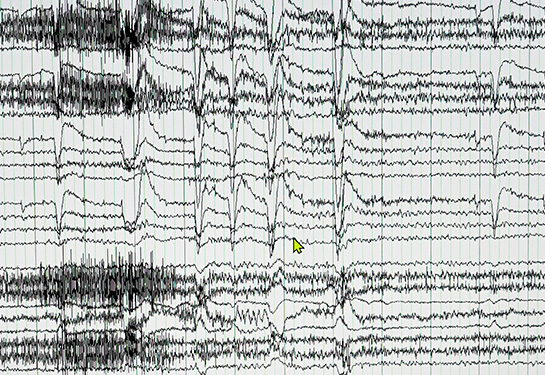
This medical detective work is completed in an epilepsy monitoring unit. Many patients experience this evaluation in two phases. In the first, electrodes are attached to the scalp to monitor seizure activity.
David Brandman is an assistant professor of neurological surgery. “A seizure is like a forest fire,” Brandman said, “in that it begins from one or more specific locations and then spreads across the brain.”
If seizures are detected and meet the requirements for treatment through surgery, the patient moves on to the second phase. At that time, their brain is temporarily implanted with a set of a dozen or so very small electrodes.
Each electrode collects electrical impulse data. The patient then stays in the monitoring unit for as long as it takes for them to experience a seizure. Once the seizure source is successfully mapped in the brain and the seizure type determined through electrode readings, the electrodes are removed. The patient goes home until their treatment surgery.
A seizure is like a forest fire, in that it begins from one or more specific locations and then spreads across the brain.”—David Brandman
Team-based care supports patients, creates research opportunities
Alongside the new expanded adult unit are four beds dedicated to monitoring epilepsy in children.
Amy Brooks-Kayal, professor and chair of neurology, specializes in pediatric epilepsy. She researches how the brain changes when epilepsy develops and how these changes can be targeted for new treatments.
Brooks-Kayal noted that UC Davis Health provides leading-edge comprehensive epilepsy care across patients’ lifespans by bringing pediatric and adult multidisciplinary specialists together in the same program.
“As one of few programs nationwide to offer this continuity and convenience to patients, our integrated team-based approach also accelerates diagnosis and treatment planning for Northern California patients with unmet neurological needs,” Brooks-Kayal said.
Care and research in the same unit
Ashley Holden lives in Roseville, California, where she and her husband parent two young children. Holden had the unique experience of initially staying in the previous UC Davis monitoring unit and then being transferred to the new one the day it opened.

“The new unit is very comfortable, including the accommodations for my husband as my support person,” Holden said. “We’re talking about surgical options for me, and the idea of any procedure on a person’s brain can be frightening. I feel more secure and confident in my future, knowing a whole team is discussing my case and preparing the plan that’s best for me.”
Beyond undergoing diagnostics, some patients participate in research while they stay in the unit.
Jack Lin, a professor of neurology and director of the UC Davis Comprehensive Epilepsy Program, combines patient care with research. He is excited about how many studies use the implanted electrodes to record, for example, how a single brain cell responds during everyday activities such as talking with your family.
“In addition to improving treatment for epilepsy, patients implanted with intracranial electrodes allow us to better understand the basic mechanisms of learning, memory, emotion and language. We can use this information to develop better treatments for different types of cognitive dysfunction,” Lin said.
Learn more about the UC Davis Comprehensive Epilepsy Program.
Related links: