Shafikhani Research Lab
 Sasha Shafikhani, Ph.D.
Sasha Shafikhani, Ph.D.
Professor and Director of Microbiome Research
Department of Dermatology, School of Medicine
University of California, Davis
3301 C St., Suite 1400, Sacramento, CA 95816
Sasha Shafikhani completed his undergraduate and doctoral studies at the University of California, Berkeley, followed by a postdoctoral fellowship at the University of California, San Francisco. He is currently a professor and the director of microbiome research in the Department of Dermatology at UC Davis School of Medicine. Shafikhani has served on the editorial boards of 13 scientific journals and is currently an associate editor for Frontiers in Microbiology and Scientific Reports.
Additionally, he has contributed to grant evaluation panels for prominent organizations such as the National Institutes of Health (NIH), NASA, and various national and international research funding agencies. As a cellular microbiologist, Shafikhani leads research projects focusing on host and pathogen interaction, normal and chronic wound healing, and cancer biology. His research has been supported by grants from NIH, philanthropic funds and institutional grants.
As a cellular microbiologist, my research focuses on applying knowledge derived from pathogen studies to advance our understanding of host cellular mechanisms. My lab is highly multidisciplinary in nature, and our research has been supported by grants from the National Institutes of Health (NIH), philanthropic funds, and institutional grants.
Research Focus
- Determine the virulence mechanisms that mediate pseudomonas aeruginosa pathogenesis in the context of wound infection
- Determine the eukaryotic host responses that are intended to control pseudomonas aeruginosa wound infections
- Develop novel antibiotic-free therapeutics to control surgical site infection
- Employ bacterial toxins as molecular tools to dissect important mammalian cellular processes such as cytokinesis, apoptotic program cell death and apoptotic compensatory proliferation signaling
Current Research Projects
Molecular dissection of impaired infection control and impaired healing in diabetic wounds
Diabetic foot ulcers are the leading cause of lower extremity amputations in the U.S. and are responsible for more hospitalizations than any other complication of diabetes. The sheer number of diabetic ulcers that progress to amputation underscores the inadequacy of conventional therapies and the need for novel approaches. This project addresses well-recognized co-morbidities associated with impaired healing in diabetic ulcers — namely, enhanced bacterial infection and microbiome shift toward pathogenic bacteria, such as Pseudomonas aeruginosa (Pa). The mechanism(s) underlying these effects remain poorly understood. Funded by an R01 grant, we are investigating why diabetic wounds fail to control infection and exhibit impaired healing. We have published extensively in this area. For example, we published a paper (Roy, et, el, 2022, eLife) demonstrating that delay in neutrophil response renders diabetic wounds vulnerable to infection. We showed how impaired chemotactic signaling through the FPR receptors (which mediates the initial wave of neutrophil chemotaxis) is responsible for this delayed neutrophil response in diabetic wounds. These studies have led to new discoveries in the lab, which are the basis for another RO1 grant.
In another example, we published a manuscript (Roy, et, al, 2022, Journal of Investigative Dermatology), in which we demonstrated that global insufficiency in the expression of pro-inflammatory cytokines, due to impaired signaling through the Toll Like Receptors (TLRs), in diabetic wounds early after injury, leads to delayed macrophage responses and causes impaired healing in diabetic wounds. We showed that increased expression of IL-10 is responsible for dampened TLR signaling. We further showed that blocking IL-10 signaling topical treatment with anti-IL10 or anti-IL10R antibodies restores TLR signaling, enhances the expression of pro-inflammatory cytokines, restores the macrophage responses, and substantially improves healing in diabetic wounds.
Developing antibiotic-free antimicrobials to control surgical site infections (SSIs)
Despite many advances in infection control practices – including improved operating room ventilation, barriers, sterilization methods, and improved surgical techniques – surgical site infection (SSI) remains a significant cause of morbidity, prolonged hospitalization, and death with a mortality rate of ~3% and an estimated annual cost of $3.5 to $10 billion in health care expenditures in the U.S. alone. It is not surprising that the U.S. Department of Health and Human Services has identified combating SSI as a top national priority. Administration of prophylaxis antibiotics in the perioperative period (~1-2 hours prior to surgery) is the standard of care for most surgical procedures. However, even short-term antibiotic use is associated with the emergence of resistance, increased risk for clostridium difficile infection, and immunological and neurological diseases — many of which have been attributed to dysbiosis in the gut flora due to antibiotics. Of note, prophylaxis antibiotics are significantly less effective in immunocompromised patients, thus highlighting the need for antibiotic-free novel approaches to control SSI. We received an RO1 grant to develop novel immunomodulator-based therapies as potential replacement or augmented therapies to prophylaxis antibiotics. We published three manuscripts (Roy et al, 2024, J. Inves. Dermatology, Mahmud et al, 2022, FASEBJ & Hamilton et al, 2021, European Cells & Materials) which demonstrate that our immunomodulator-based approaches are as effective (if not more) as systemic antibiotics in controlling P. aeruginosa and MRSA surgical site infections in wounds and in periprosthetic joint implant. These data have also resulted in several approved and pending patents.
Determining virulence strategies that Pseudomonas aeruginosa to evade innate immune defenses
Funded by NIH R21 and RO1 grants, we have assessed many virulence strategies that facilitate the pathogenesis of Pseudomonas aeruginosa and host innate immune responses that can recognize and combat this pathogen. As an example, we recently published a paper in (Mohamed et al, 2022, Nature Communications) which demonstrated that P. aeruginosa recognition by host innate immunity involves the recognition of its Type III Secretion System which leads to a phosphorylation cascade through CrkII/Abl › PKCδ › NLRC4, culminating in caspase-1 canonical inflammasome activation which combats P. aeruginosa infection in wounds. Through these studies, we were able to identify and characterize CrkII adaptor protein and Abl tyrosine kinase as new essential components of the NLRC4 inflammasome.
Role of Apoptotic Compensatory Proliferation Signaling (ACPS) in wound healing, cancer, and in innate immunity against invading pathogens
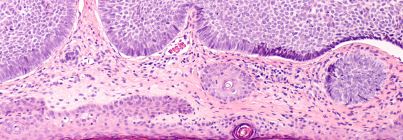
In addition to its role in Programmed Cell Death (PCD) - apoptosis has also been implicated in triggering Compensatory Proliferation Signaling (CPS), whereby dying cells induce proliferation in neighboring cells as a means to compensate for their own demise. The underlying mechanism of CPS has remained largely unknown. One research area in our laboratory has been to determine the mechanisms by which P. aeruginosa induces apoptosis in target host cells. During these studies (published in PLoS Pathogens and JBC), we serendipitously discovered the mode of communication between apoptotic cells and their neighboring cells that is responsible for CPS. In a recent publication in Developmental Cell (Gupta et al, 2017), we reported that under apoptotic — but not necrotic — conditions, primary and transformed epithelial cells produce and release specialized microvesicles, which stimulate compensatory proliferation in surrounding bystander cells upon contact. We have purified these microvesicles, both in vitro and in vivo, and termed them ACPSVs (Apoptotic Compensatory Proliferation Signaling Vesicles). Our Scanning Electron Microscopy (SEM) and Differential Interference Contrast (DIC) imaging, as well as, our time-lapse videomicroscopy and biochemical data indicated that ACPSVs are distinct from previously described exosomes and apoptotic bodies. For the first time, we provided visual evidence of CPS and showed by live videomicroscopy how ACPSVs are generated and released from apoptotic cells prior to their death and how they induce proliferation both in primary and transformed cells upon contact. We have extended these studies to assess the occurrence of ACPSVs in health and disease. Our preliminary data indicate that these vesicles are produced by all cancer cells and in solid tumors (Mohamed et al, 2022, Scientific Reports). Intriguingly, we have also found that P. aeruginosa Exotoxin T (ExoT) blocks vesicle production while inducing potent apoptosis, thus uncoupling apoptotic PCD from apoptotic CPS. These data further suggest that CPS could be deleterious to P. aeruginosa pathogenesis and blocking CPS could benefit P. aeruginosa during infection.
See all publications by Shafikhani »
Ruchi Roy, Foyez Mahmud, Janet Zayas, Timothy M. Kuzel, Jochen Reiser, & Sasha H. Shafikhani. Reduced Bioactive Microbial Products (PAMPs) Contribute to Dysregulated Immune Responses And Impaired Healing in Infected Wounds in Diabetic Mice. Journal of Investigative Dermatology. 2024, Feb;144(2):387-397.e11. PMID: 37619833. PMCID: PMC10840742; DOI: https://doi.org/10.1016/j.jid.2023.08.004.
Mohamed F. Mohamed, Kajal Gupta, Josef W. Goldufsky, Ruchi Roy, Lauren T. Callaghan, Dawn M. Wetzel, Timothy M. Kuzel, Jochen Reiser & Sasha H. Shafikhani. CrkII/Abl phosphorylation cascade is critical for NLRC4 inflammasome activity and is blocked by Pseudomonas ExoT. Nature Communications. 2022 Mar 11. 13(1):1295. doi: 10.1038/s41467-022-28967-5. PMID: 35277504. PMCID: PMC8917168.
Ruchi Roy, Janet Zayas, Sunil K. Singh, Kaylee Delgado, Stephen J. Wood, Mohamed F. Mohamed, Dulce M. Frausto, Yasmeen A. Albalawi, Thea P. Price, Ricardo Estupinian , Eileena F. Giurini, Timothy M. Kuzel, Andrew Zloza, Jochen Reiser, & Sasha H Shafikhani. Overriding impaired FPR chemotaxis signaling in diabetic neutrophil stimulates infection control in murine diabetic wound. eLife. 2022, Feb 3. 11:e72071. doi: 10.7554/eLife.72071. PMID: 35112667. PMCID: PMC8846594.
Ruchi Roy, Janet Zayas, Mohamed F. Mohamed, Mohammad Bayat, Timothy M. Kuzel, Jochen Reiser & Sasha H. Shafikhani. IL-10 Dysregulation underlies Global Chemokine Insufficiency, Delayed Macrophage Response, and Impaired Healing in Diabetic Wound. Journal of Investigative Dermatology. 2022 Mar. 142(3 Pt A):692-704.e14. doi: 10.1016/j.jid.2021.08.428. Epub 2021 Sep 10. PMID: 34517005. PMCID: PMC8860852.
Kajal H. Gupta, Josef W. Goldufsky, Stephen J. Wood, Nicholas J. Tardi, Gayathri S. Moorthy, Douglas Z. Gilbert, Janet P. Zayas, Eunsil Hahm, Mehmet M. Altintas, Jochen Reiser, & Sasha H. Shafikhani. Apoptosis and compensatory proliferation signaling are coupled by CrkI-containing microvesicles. Developmental Cell. 2017, Jun 19. 41(6):674-684.e5. PMID: 28633020, PMCID: PMC5533184. doi: 10.1016/j.devcel.2017.05.014.