Since 2005, the Extracorporeal Life Support Program at UC Davis Health has delivered advanced, lifesaving care for patients of all ages with severe heart or lung failure.
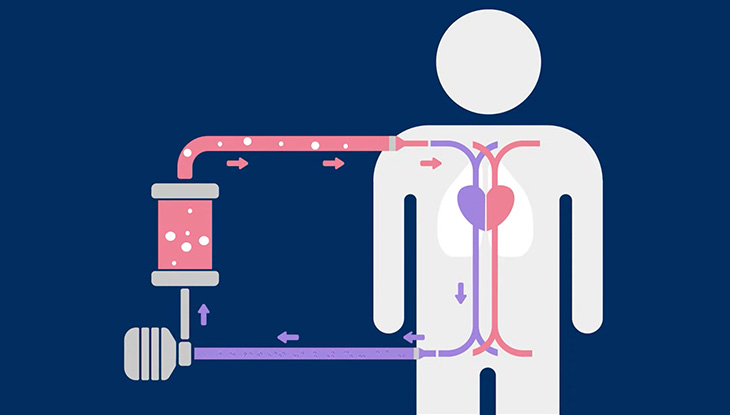
Using extracorporeal membrane oxygenation (ECMO), we support critically ill neonates, children, and adults when conventional therapies are no longer enough. Our multidisciplinary team of intensivists, surgeons, perfusionists, and nurse ECMO specialists work with UC Davis Health’s comprehensive services to provide 24/7 rapid ECMO deployment, continuous bedside care, and coordinated support across the lifespan as a bridge to recovery, transplant, or long-term therapies.