Neurosurgery, maternal-fetal medicine team save pregnant woman of risky spinal fluid cyst
Empowered by knowledge and guided by expert care, Darlene Hildebrandt navigated a complex pregnancy
A few weeks before Thanksgiving, Darlene Hildebrandt and her husband welcomed their first child. They may never have met their healthy baby boy, and Hildebrandt herself may have faced life-threatening risks, had they not been referred to UC Davis Health earlier this year. She found the right high-risk obstetrics and neurosurgical care team to understand her very unique medical situation.
‘I gave up hope’
In 2015, Hildebrandt, who was 24 years old, learned she had a rare variant of spina bifida, a congenital medical condition.
She was born with an incompletely formed sacrum (the base of the spinal column) with abnormal openings in the bone. The covering of her spinal cord, or the meninges, pushed through one of these openings, allowing spinal fluid to collect into a growing cyst in her pelvis.
This type of cyst is called an anterior sacral meningocele (ASM). It affects only one in 100,000 people worldwide, mostly women.
At that time, Hildebrandt ’s ASM was a modest size. Doctors recommended leaving it alone.
Seven years later, Hildebrandt and her husband started planning for a baby. At her gynecologist’s office in Chico, Darlene learned the cyst had grown quite large. In addition, imaging showed her uterus appeared unusually shaped. She was referred to a group of top adult spine neurosurgeons in California.
“After two years of evaluation, they had nothing to offer me,” Hildebrandt said. “I gave up hope for treatment.”
Hildebrandt ’s impression from the outside spine specialists was that getting pregnant would pose no unusual risk, because she was told the ASM would be pushed safely back into her spinal canal as the developing baby grew. “They made it seem like it wasn’t a big deal,” she recalled.
Pregnant and in danger
In spring 2025, Hildebrandt was delighted to discover she was pregnant. Yet, she worried how her unresolved health condition would affect her developing baby, and whether pregnancy would be risky for her.
Her local gynecologist referred Hildebrandt to the Maternal Fetal Medicine clinic at UC Davis Health, where she met Leanna Sudhof, a physician specializing in high-risk pregnancies in the Department of Obstetrics and Gynecology. Hildebrandt was a little over 14 weeks pregnant.
The doctor quickly discovered this was an extraordinarily rare and complex pregnancy.
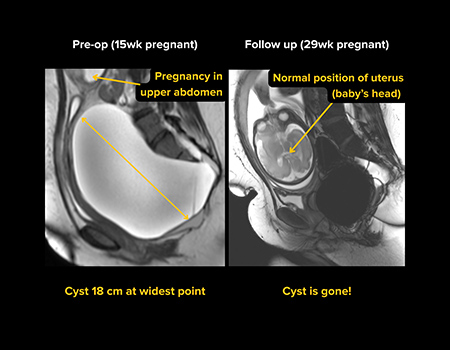
“When I first saw her in clinic, I was amazed by what our bedside ultrasound revealed. I had never encountered anything like it,” said Sudhof, an experienced maternal-fetal medicine specialist. “The ASM was huge, filling Darlene’s entire pelvis, and the uterus was displaced up high under her ribs. The vagina and cervix were very elongated, crossing over the massive cyst to connect to her uterus.”
Hildebrandt and Sudhof found themselves in a serious situation: “I was seeing case reports of these rupturing spontaneously as the uterus grows, which introduces the risk of meningitis and other more serious outcomes, including death,” Sudhof said.
Husband and wife team to the rescue
Lucky for Hildebrandt and her developing baby, Sudhof knew just the colleague to help with this rare case. And she happens to be married to him.
Sudhof admitted Hildebrandt to UC Davis Medical Center for an urgent MRI and consultation with pediatric neurosurgeon Cameron Sadegh.
“These days, most forms of spina bifida are diagnosed before or shortly after birth and are treated by pediatric neurosurgeons like me,” Sadegh said.
ASMs, however, are usually diagnosed later in life. The UC Davis pediatric neurosurgery team treats congenital neurological malformations like spina bifida across the lifespan because they are considered pediatric diagnoses.
Sadegh explained Hildebrandt ’s condition in careful detail and guided her through the surgery he intended to perform. First, he would make a small bony window in the back of the sacrum, well below the bottom of the spinal cord.
Through this window, Sadegh would check for any nerve roots involved in the cyst. Then he would disconnect the fibrous band that was tethering the large cyst to Hildebrandt ’s spinal cord. Lastly, he would tie off, or ligate, the neck of the cyst to prevent it from reforming in the future. Sadegh was confident this approach would work for Hildebrandt.
Hildebrandt, Sadegh and Sudhof determined that the best way forward was to operate on the ASM as soon as possible, to prevent future harm to Hildebrandt and save her developing baby.
‘The scariest moment of my life’
“I’d never had surgery before, but Dr. Sadegh was so self-assured and positive. He was realistic about the risks but not scared of them. He was confident my baby and I would be fine,” Hildebrandt said.
She felt nervous. But she was determined to become a mother, and she wanted this baby. She agreed to return to Sacramento that same week for surgery.
“Making this decision was the scariest moment of my life,” Hildebrandt confessed. “I felt the baby kick during the MRI. Even though I trusted Drs. Sadegh and Sudhof, I was really afraid my baby wouldn’t make it.”
Sudhof and Sadegh teamed up to take care of Hildebrandt and her developing baby. Sadegh performed the surgery as planned. It was an immediate success.
In the operating room, Sudhof used ultrasound to check Hildebrandt’s uterus and organs after the surgery. She saw that the organs were already settling into normal positions. The developing baby survived the long operation.
The repair to Hildebrandt’s meninges also held strong in the days after. She soon returned home for the remainder of her pregnancy.
Knowledge is power and leads to safe delivery
During the surgery, Hildebrandt also underwent a detailed pelvic exam to understand the unique anatomy of her uterus. This exam helped in planning the rest of the pregnancy and delivery.
Sudhof confirmed that Hildebrandt’s uterus is bicornuate, which is Latin for “two horns.” A bicornuate uterus is shaped like a heart, with an indentation at the top where a uterus would commonly be rounded. Only about 0.4% of girls are born with this condition — but as many as half of women with ASM have it.
“These reproductive tract differences in development are part of a group known as Mullerian anomalies and they happened when Hildebrandt was in her own mother’s womb,” Sudhof explained.
“I wish other providers I saw shared their findings about my body with me the way Sudhof and Sadegh have,” Hildebrandt said.
While many people with Mullerian anomalies safely deliver healthy babies, it’s still a risk factor for other complications, specifically preterm labor — which Hildebrandt experienced one night in November.
A healthy boy is born

At almost 33 weeks, Hildebrandt’s water broke. Sudhof urged her to travel to UC Davis Medical Center by air ambulance.
Two days later, her son arrived through an uncomplicated delivery. He was transferred to the neonatal intensive care unit, where he spent several weeks while his lungs fully developed and he gained weight.
The baby boy went home earlier than expected, giving the family plenty of time to prepare for cozy winter celebrations.
“We’re doing great!” Hildebrandt said. “We enjoyed a low-key first holiday season with immediate family.”




