New hope for patients with head and neck cancer
UC Davis scientists use federal research grant to test three-prong cure for head and neck cancer that includes a common blood pressure drug
Head and neck cancers are among the most difficult to treat. They can be aggressive and are located near some of the body’s most vital areas: nose, mouth, throat. Chemotherapy and radiation have been the primary weapons against tumors that cannot be surgically removed, but the results in advanced cancers have been poor.
Immunotherapies have great potential to improve this landscape. These drugs recruit immune T cells to attack tumors — harnessing the body’s preexisting defense mechanisms to defeat cancer. Unfortunately, this approach is also a work in progress.
But now, researchers at UC Davis Comprehensive Cancer Center have initiated an innovative clinical trial to provide better results against head and neck cancers. It combines the immunotherapy drug pembrolizumab, also known as KEYTRUDA, and a commonly prescribed blood pressure medication losartan, sold as COSAAR, with a new therapeutic radiation. Stereotactic body radiation therapy (SBRT) is different than conventional radiation in that it uses multiple beams of energy to shrink tumors.
“Immunotherapy has shown so much promise in other cancers, but it hasn’t been particularly effective against head and neck cancer,” said cancer center Chief Science Officer Xiao-Jing Wang. “We’re hoping this combination of radiation, losartan and immunotherapy can provide better results for patients.”
How it all started
Wang joined UC Davis Comprehensive Cancer Center in 2022, bringing with her a $9.8 million Specialized Programs of Research Excellence (SPORE) grant received from the National Cancer Institute (NCI). She was previously at the University of Colorado when she and her team were awarded the SPORE grant.
Using the SPORE grant, Wang began to study how immunotherapy could be used more effectively against head and neck tumors — one of only three SPORE grants for this type of cancer.
This research started with preclinical studies that tested radiation, immunotherapy and drugs that limit TGF-β, a protein that slows down the body’s defense system. After setbacks regarding clinical development for TGF-β inhibitors, the team adopted losartan, which also inhibits TGF-β.
Most head and neck cancer patients are men over 60 who smoke. Not surprisingly, these patients also face high blood pressure. Clinicians have observed that patients taking losartan seem to respond better to radiation. This and other clues led the team to the blood pressure drug.
“We realized we could repurpose losartan, a drug that has a well-established safety profile, to help cancer patients,” said Wang. “It could control their blood pressure and suppress TGF-β, which could make immunotherapy more effective.”
Moving the research from the lab into the clinic
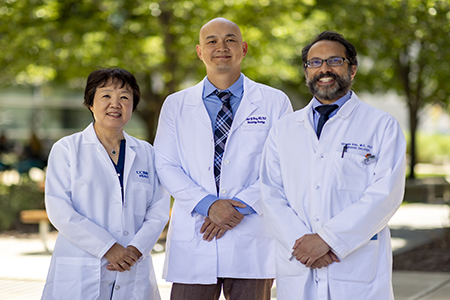
SPORE grants are designed to fund both lab and clinical research. This unique mechanism helps ensure that successful discovery work is translated into clinical care. Wang recruited cancer center clinical investigators Shyam Rao, professor, Department of Radiation Oncology, and Siao-Yi Wang, assistant professor, Division of Hematology and Oncology, to help conduct the phase 1b safety trial.
The study is delivering the three-pronged treatment to patients with locally recurrent head and neck carcinomas. These patients were previously treated for the disease but their cancer has returned.
“If patients fail their initial curative treatments and have recurrences or metastases, there aren’t many good treatments,” said Rao. “We have cytotoxic chemotherapies, which can slow things down, but they’re pretty rough. We want to expand that toolbox.”
Radiation and the abscopal effect
The trial is using SBRT to target metastases. SBRT focuses increased doses of radiation to kill recurrent tumors while narrowing the target so it is gentler on patients. The risk is that the radiation will miss tiny cancer cells too small to see on scans that could eventually form new tumors.
To lessen that concern, oncology teams have traditionally relied on chemotherapy, a systemic treatment. Immunotherapy could perform the same role but with fewer side effects. The key is making it more effective.
Radiation is known to increase TGF-β, suppressing the immune response. On the other hand, there’s the Abscopal effect, in which untreated tumors in distant parts of the body shrink on their own. The hypothesis is that irradiated tumor cells die, releasing proteins that prime the immune system and generate a vaccine-like effect against untreated tumors. However, if the radiation is boosting TGF-β and suppressing immunity, there may not be enough of these cytotoxic T cells or “killer T cells” to effectively do the job.
“Dr. Wang’s research has shown us losartan suppresses TGF-β in head and neck cancer, which may free up the immune system to better respond to tumors and hopefully any micro metastases,” said Rao. “This could make the radiation and immunotherapy combination more effective.”
Passing early tests
The cancer center trial, which recently expanded to the University of Colorado Cancer Center, is primarily testing the safety of the new therapy. So far, the study has treated seven patients, six at UC Davis, and early results are encouraging.
“All the patients seem to be handling the treatment well,” said Rao. “While safety is the primary study point, we’ve also seen tumors shrink. But the proof comes in time, we have to follow up for a year or two to make sure this approach is truly working.”
Looking past this current study, Rao and colleagues believe their research could open a new therapeutic pathway and give patients more options.
“This and subsequent trials may show us that TGF-β inhibition, through losartan, enhances the efficacy of both SBRT and immunotherapy,” said Rao, “However, there may be other TGF-β inhibitors that are even more effective than losartan. This work could open the door to finding those agents.”
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.