Study uncovers how chronic kidney disease impacts glucose and glycemic control
A new collaborative study from researchers at UC Davis Health and the UC Davis School of Veterinary Medicine reveals how complications from chronic kidney disease (CKD) are linked to problems in the metabolic system.
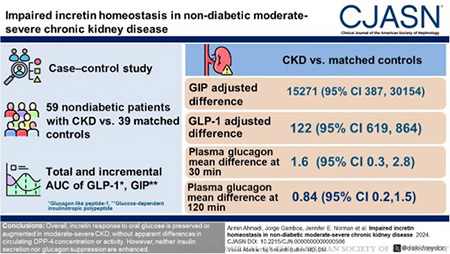
The study, published in the Clinical Journal of the American Society of Nephrology, looked at incretin hormone levels in patients with kidney disease and compared them to those without kidney disease. It found that incretin hormones glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) were higher in patients with kidney disease. However, those higher levels of incretin did not result in an enhanced insulin secretion as they did with healthy patients.
This physiological dysregulation could signal an interplay in patients who have kidney disease and other chronic conditions like cardiovascular disease, diabetes and obesity, which are highly prevalent in this population.
What the study showed
The researchers performed a two-hour oral glucose tolerance test on 59 non-diabetic individuals with moderate to severe kidney disease and 39 controls. The groups were matched for age, sex and race. All the participants were given a 75-gram oral glucose test.
The team collected blood samples from the participants at various time points during the two-hour period. With the blood tests, they measured several hormones, including GLP-1, GIP, C-peptide, insulin, glucose and glucagon. They also estimated the hormone secretion during this period.
Researchers found that patients with CKD had higher levels of GLP-1 and GIP compared to controls throughout the test period.
“This data is significant because it is the first robust evidence we have seen that shows what happens to GLP-1 and GIP levels in non-diabetic patients with moderate to severe kidney disease after they have a meal,” explained Armin Ahmadi, postdoctoral scholar of nephrology at UC Davis Health and lead author of the study. “But we were also curious about how GLP-1 and GIP impacted insulin and glucagon secretion.”
Researchers were surprised to find there were no differences with glycemic control even though the kidney disease patients were secreting more GLP-1 and GIP. Their results also showed that glucagon was higher in kidney disease patients despite their insulin levels being the same.
“This showed us that GLP-1 and GIP are not as effective in shutting down glucagon and stimulating insulin secretion in patients with kidney disease compared to controls, suggesting increased resistance to their action in CKD,” Ahmadi added.
No differences in DPP-4
Another novel finding researchers discovered involved the enzyme dipeptidyl peptidase-4 (DPP-4), which breaks down GLP-1 and GIP after they are secreted.
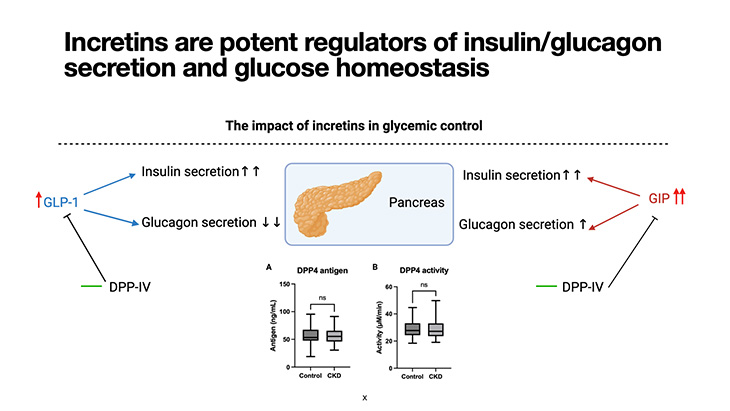
“We wanted to know if the higher levels of GLP-1 and GIP were due to higher secretion or if they were due to less DPP-4-mediated breakdown of these two hormones in patients with kidney disease,” explained Lars F. Berglund, distinguished professor emeritus of endocrinology and coauthor of the study.
Researchers found no differences in the levels of DPP-4 in the patients with kidney disease and the healthy individuals. This means that the higher levels of GLP-1 and GIP were due to the hormones being secreted more and not being broken down by DPP-4.
“This is important because it may suggest patients with kidney disease have an inherent resistance to these hormones and that medications like Ozempic or Mounjaro that boost the effects of GLP-1 and GIP may be of particular benefit to those who tolerate them,” Berglund added.
Next steps
The researchers noted that there is much more work to do around this topic.
“This discovery gives us a basic understanding of how having kidney disease impacts cardiometabolic health by increasing resistance to the effects of these important hormones,” explained Baback Roshanravan, professor of nephrology and a senior investigator on this project. “This basic understanding could provide us with a path to better treating cardiovascular-kidney-metabolic syndrome in patients living with kidney disease.”
UC Davis coauthors of the study include Brian J. Bennett, Enkhmaa Byambaa, Bethany Cummings, Sili Fan, Jennifer E. Norman and Madelynn Tucker and researchers from the University of Washington Kidney Research Institute.
Learn more about our diabetes and endocrinology expertise.




