Clinical trial may offer relief for rare autoimmune disease
Study involving UC Davis Health published in the New England Journal of Medicine shows progress in treating primary biliary cholangitis
A clinical trial involving UC Davis Health suggests the investigational drug Seladelpar is a potential novel treatment for patients with the rare, autoimmune disease primary biliary cholangitis. The drug helped reduce cholestasis and liver injury, and led to significantly less itching for patients.
The results of the clinical trial were published in The New England Journal of Medicine.
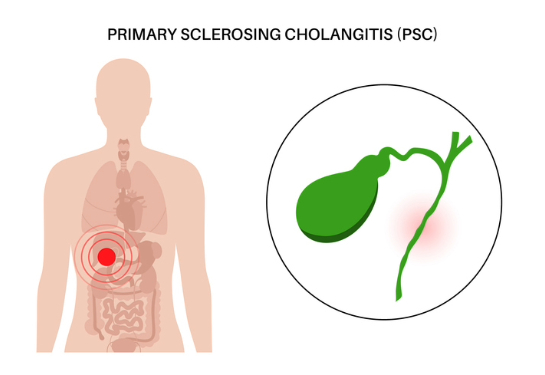
Primary biliary cholangitis is a disease that damages the bile ducts in the liver and can lead to liver failure. It slowly degrades the ducts, which makes it harder for bile to flow from the liver, which in turn further damages the liver.
Most patients with primary biliary cholangitis experience fatigue and itchy skin, which can be debilitating.
“For many patients living with primary biliary cholangitis, there is not a treatment that offers meaningful symptom relief,” said Christopher Bowlus, chief of Gastroenterology and Hepatology at UC Davis Health and co-author of the paper. “New options, that are potent, effective and safe, are needed for people living with this chronic debilitating autoimmune condition.”
RESPONSE clinical trial
As many as 40% of patients with primary biliary cholangitis have an inadequate response to the traditional first-line therapy of naturally occurring ursodeoxycholic acid. These patients are at a high risk for disease progression, and more than half fail to respond to the second-line therapy, obeticholic acid.
The phase 3 RESPONSE trial took place at UC Davis Health and other sites. A total of 193 patients with primary biliary cholangitis who had an inadequate response to — or who could not tolerate ursodeoxycholic acid — were randomly given either 10 mg. of Seladelpar or a placebo, once daily for 12 months. Most patients (93.8%) continued ursodeoxycholic acid as standard-of-care therapy during the trial.
The goal was to achieve a biochemical response, defined as an alkaline phosphatase (ALP) level greater than 1.67 times the upper limit of the normal range, with a decrease of 15% or more from baseline. Researchers also sought a normal total bilirubin level, which is associated with better long-term survival, free of liver transplantation. After 12 months, 61.7% of patients taking Seladelpar met the primary endpoint, which was achieved by only 20% of patients taking placebo.
“This treatment has the potential to both effectively manage the disease progression and improve the burden of a patient’s symptoms.” —Christopher Bowlus
In addition, significantly more patients taking Seladelpar (25%) than placebo (0%) had a normalization of the ALP level. The average decrease in ALP from baseline was 42.4% in the Seladelpar group versus 4.3% in the placebo group.
A key secondary result was a change in patient-reported itching. At the beginning of the trial, 38.3% of patients in the Seladelpar group and 35.4% of those in the placebo group reported moderate to severe itching.
The patients in the Seladelpar group experienced a significant reduction in itching compared with the placebo group. These improvements were sustained through 12 months.
“The data in this trial shows people living with primary biliary cholangitis saw substantial rates of normalization of serum liver tests and clear statistically significant improvement in itch,” explained Bowlus. “This treatment has the potential to both effectively manage the disease progression and improve the burden of a patient’s symptoms.”