Surgery may benefit macular edema from Coats disease
Earlier surgical intervention for advanced cases may result in better vision
Surgical drainage of large macular cysts in a patient with Coats disease resulted in an immediate resolution of edema and a gradual resolution of lipid exudates over one year. However, visual recovery was limited due to the chronic nature of the condition. Earlier surgical intervention, in some cases, may allow for visual rehabilitation.
Those findings come from a new case study by ophthalmologists at the UC Davis Ernest E. Tschannen Eye Center published in the Journal of VitreoRetinal Diseases.
“For some patients with macular Coats disease that does not improve with standard treatments like laser injections and intraocular injections, surgically draining the large cysts may be a viable alternative,” said Glenn Yiu, first author of the paper and a professor and board-certified vitreoretinal specialist and surgeon at UC Davis.
Coats disease characterized by abnormal blood vessels
Coats disease is a rare, idiopathic eye disorder characterized by abnormal development of blood vessels in the retina. It is usually diagnosed in childhood. The progressive disease occurs three times more frequently in males than females and generally presents in only one eye. Early symptoms can include decreased visual acuity, strabismus and leukocoria, where the eye’s pupil reflects white, grayish or yellowish instead of red.
Patients with Coats disease can present with large amounts of cystoid edema and lipid exudates in the retina, which can severely impair vision if they develop in the macula — the central part of the retina needed for reading or recognizing faces.
For some patients with macular Coats disease that does not improve with standard treatments like laser injections and intraocular injections, surgically draining the large cysts may be a viable alternative.” —Glenn Yiu, professor, Department of Ophthalmology and Vision Sciences
Large macular cystoid spaces
A 30-year-old man with Coats disease was referred to the Eye Center at UC Davis Health. He was diagnosed with the disease at age 9 and initially received multiple rounds of laser photocoagulation to eliminate the abnormal vessels and leaking aneurysms. His left eye had become blurrier over several years as the macular edema and exudates progressively worsened.
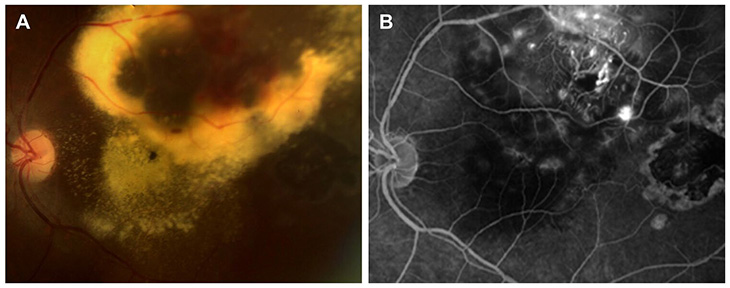
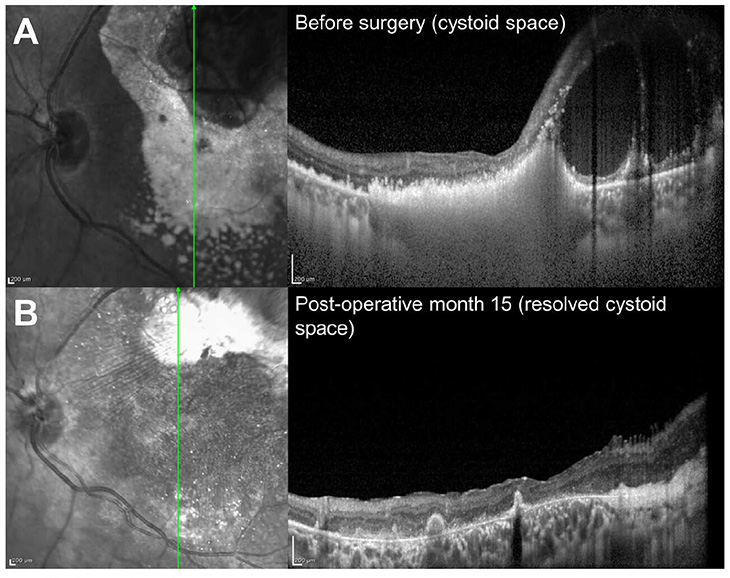
At the time of his referral, the vision in his affected eye was 20/400, with large macular cysts seen on fundus examination and optical coherence tomography (OCT). OCT is a type of imaging retinal specialists commonly use to see the retina in cross-section and detect microscopic pathologic changes.
Using fluorescein angiography to visualize retinal blood flow, Yiu also noticed active leakage from these telangiectasias and aneurysms. The patient was initially treated with additional laser photocoagulation and multiple rounds of anti-vascular endothelial growth factor (anti-VEGF) injections to stop the leakage, but without success.

Surgical drainage and laser photocoagulation
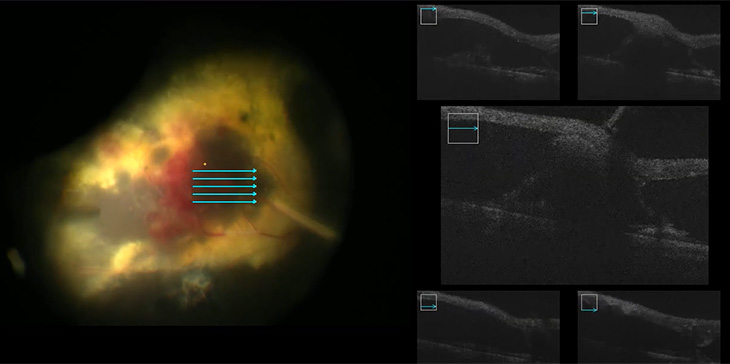
After extensive discussions with the patient, ophthalmologists decided to attempt surgical drainage as a last resort. Yiu and his team performed a pars plana vitrectomy (PPV) to remove the vitreous. Then, using intraoperative OCT imaging for guidance, they created a retinal opening called a retinotomy, and successfully drain the large cysts and lipid exudates using a microscope aspiration cannula. They sealed the retinal opening and treated all the aneurysms with intraocular laser photocoagulation, or endolaser”.
They performed intraoperative OCT again to confirm the complete removal of the fluid at the completion of the case.
Postoperative OCT images captured one month after the surgery showed no fluid recurrence in the eye and some reduction in subfoveal exudates. After one year, the lipid exudates had disappeared as well, although the patient’s vision remained unchanged at 20/400.
“This case shows the possibility of surgically draining large macular cysts in cases of advanced Coats disease refractory to medical intervention,” said co-author Abraham Hang, a third-year resident in the UC Davis Department of Ophthalmology and Vision Science.
The authors note that based on the resolution of the macular fluid and exudates after surgery, perhaps earlier surgical intervention could have resulted in better vision outcomes. “Chronic macular fluid and especially lipid exudates are very toxic to the retina,” Yiu noted.
However, they caution that potential complications related to intraocular surgery should be carefully considered, and optimal care with conventional laser photocoagulation and intravitreal injections should be prioritized.
“Careful consideration of the surgical risks must be weighed against the potential benefit of treating the macular fluid and exudates in a timely manner,” Yiu said.
Resources
The UC Davis Eye Center
The UC Davis Eye Center provides world-class eye care, pioneers collaborative vision research, and trains the next generation of specialists and investigators to become leaders in the Sacramento region and beyond. The Eye Center team aims to transform vision care and develop cures for blinding eye diseases, from cornea to cortex.