UC Davis Health receives $2.8 million grant from NIH to create AI-based digital pathology tool
Researchers will analyze cell therapy for treatment of chronic inflammatory conditions
UC Davis Health gastroenterology researchers have received a $2.8 million grant (R01EB037526) from the National Institute of Biomedical Imaging and Bioengineering (NIBIB) of the National Institutes of Health (NIH) to study the mechanisms of cell therapy using an AI-based digital pathology tool.
The four-year study will further investigate regenerative therapies, particularly using stem cells, to help treat chronic inflammatory conditions. It will also focus on how AI can assist pathologists in scoring damaged and affected tissue more quantitatively.
“We’re excited to be advancing cell-based therapies while also developing new tools to more precisely measure and assess tissue damage,” said Maneesh Dave, professor of gastroenterology and principal investigator of the study. “By deepening our understanding of these treatments, we hope to pave the way for novel therapies that could transform how chronic inflammatory conditions are managed.”
Mechanisms of cell therapy
In earlier studies, Dave and his team investigated the therapeutic effects and mechanisms of mesenchymal stem cells (MSCs) as treatments for Crohn’s disease. Their research revealed that MSCs promote sustained tissue healing through a two-stage process.
In the initial phase, MSCs release prostaglandin E2 (PGE2), a molecule that suppresses inflammatory T-cells, and reprograms macrophages (a specialized type of white blood cell) into an anti-inflammatory state. In the later phase, these macrophages engulf the dying MSCs through a process called efferocytosis, further reinforcing their anti-inflammatory behavior and prolonging the immune response.
These findings offer a compelling explanation for how stem cell therapies may work in humans and why their effects often persist longer than expected.
“With this grant, we’re exploring new questions, such as what happens if we enhance MSCs to produce more trophic factors, or whether non-viable cells alone could still provide therapeutic benefits,” Dave explained. “These are some of the exciting directions we're pursuing to deepen our understanding and advance cell-based therapies to the clinic.”
AI pathology tool
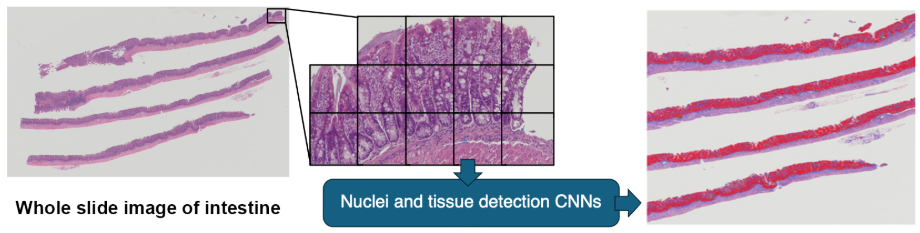
As part of the new grant, Dave will collaborate with Satish Viswanath at Emory University to develop an innovative tool called the Inflammation Digital Pathology Tool. This AI-powered platform aims to revolutionize how researchers analyze tissue samples in studies of intestinal inflammation.
The team is leveraging a collection of digitized histopathology slides from mouse models, including those used in MSC research and other studies of inflammatory bowel disease (IBD) and graft-versus-host disease (GVHD). These slides, scanned at ultra-high resolution, form a growing database of over 700 samples, with plans to expand to more than 1,000.
Traditionally, pathologists look at tissue slides and estimate how much of the area is affected. While this has long been considered the gold standard for assessing disease and treatment response, it is a time-consuming and subjective process that relies heavily on human judgement.
“There’s a critical need for development of standardized technologies that enable quantitative evaluation of histologic disease activity in animal models, thereby improving rigor, reproducibility, and translatability.”—Maneesh Dave
“We want to automate and quantify this process,” said Dave. “With digitized slides, we can measure the affected area and better assess damage — all in a consistent, objective way. There’s a critical need for development of standardized technologies that enable quantitative evaluation of histologic disease activity in animal models, thereby improving rigor, reproducibility, and translatability.”
To ensure accuracy, the team is working closely with a veterinary pathologist to validate the AI’s findings and refine the system. The hope is that the tool will not only match human-level precision but also uncover subtle patterns that the human eye may miss.
“We plan to release the tool along with our growing collection of digitized slides,” Dave added. “Our goal is to make it available to the broader research community for validation, collaboration and new discoveries.”
Additional collaborators on the grant include Richard Levenson, professor of pathology and Laboratory Medicine; William Murphy, distinguished professor of immunology; and Pedro Ruivo, health sciences clinical assistant professor.
Related article