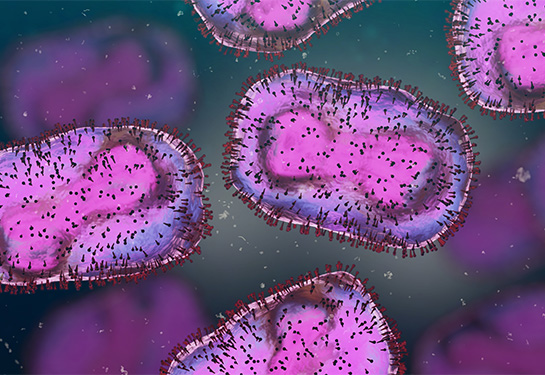
What you need to know about the latest mpox outbreak
Infectious diseases expert answers questions about a more severe and deadly type of the virus formerly called monkeypox
Mpox clade I, one of two types of the virus formerly called monkeypox, is spreading quickly in Africa. Mpox clade I causes more severe illness and death than the other type – mpox clade 2. More than 18,000 cases have been reported this year, many of them children. At least 600 deaths have been reported.
The World Health Organization declared a public health emergency of international concern last month, due to the rapid spread of mpox clade 1.
Mpox clade 1 is believed to be more infectious and more deadly than mpox clade 2, which caused the global outbreak in 2022 and 2023.
We asked Dean Blumberg, chief of pediatric infectious diseases at UC Davis Children’s Hospital, to answer questions about this latest outbreak.
What is a clade and what is the difference between clade 1 and clade 2 of mpox?
In biology, a clade is a group of organisms with a common ancestor. The World Health Organization has confirmed that there are two distinct clades of the mpox virus: clade 1 and clade 2.
Mpox clade 2 is what caused the global outbreak of mpox in 2022 and 2023.
Mpox clade 1 is what is circulating now in Africa — including African countries that haven’t reported cases of mpox in the past. As of Sept. 3, 2024, cases have also been reported in Sweden, Thailand and Pakistan after travel to Africa.
What are the signs and symptoms of mpox?
Common symptoms of both clade 1 and clade 2 mpox are:
- Rash
- Fever
- Sore throat
- Headache
- Muscle aches
- Back pain
- Low energy
- Swollen lymph nodes
For some, the first symptoms will be similar to influenza or COVID. But the development of the rash is hard to miss. See photos of the mpox rash. The lesions can appear on the hands, feet, chest, face or genitals. It starts as macules, which are flat lesions. Then it forms a firm nodule. From there, it becomes a blister, then a pustule (a blister containing pus) and then it scabs over. It can be painful or itchy. Symptoms typically last two to four weeks, but may last longer in those with weakened immune systems.
How long does it take before symptoms appear?
According to the Centers for Disease Control and Prevention (CDC), the incubation period (the time from when one is infected to when symptoms appear) for mpox is 1-21 days after exposure. During this incubation period, people who are infected may feel fine and have no symptoms. People may be contagious one to four days before symptoms appear and can stay infectious until the skin rash scabs and heals over.
How is it transmitted?
Mpox is transmitted through close person-to-person contact. This can be through talking or breathing close to one another, touching or sex and through sharing contaminated materials such as clothing or bedding (see the CDC’s tips for cleaning and disinfecting). Pregnant people can transmit the virus to their fetus. People can also contract it from infected animals, either by being scratched or bitten, or by eating meat from an infected animal.
Is there a vaccine for mpox?
Yes, JYNNEOS is a two-dose vaccine developed to protect against mpox and smallpox. It can be administered to adults or to patients under 18 years of age (but it is not part of the regular vaccine schedule for children). People need to get both doses of the vaccine for the best protection against mpox, if they have been exposed. The second dose should be given four weeks after the first dose. You can start to have an immune response after the first dose of JYNNEOS, but it takes two weeks after the second dose to be the most protected.
If the vaccine is given within four days of exposure, it protects about 85% of the time. Even if the vaccine is given up to two weeks after exposure, it may modify the disease, making it less severe.
In addition, there are some antivirals and immunoglobulins that are available to treat mpox. For patients under 6 months of age, Vaccinia Immune Globulin Intravenous (VIGIV) is an option, according to the CDC.
Is there a way to test for mpox?
If a health care provider suspects that a patient has been exposed to mpox, they can get a sample of a lesion and send it to the state for testing. If it turns out positive, the result will be confirmed at the CDC.
How do you treat mpox?
Most patients recover with supportive care and pain control.
Tecovirimat is an antiviral therapy that is available for mpox treatment. It is not yet approved by the Food and Drug Administration, and is generally used only for those with severe infection, or at risk for severe infection.
Antiviral treatment is generally given for patients with severe disease such as infection of the eye, neurologic complications, heart inflammation, mucosal lesions (occurring in the mouth, rectum, genitalia and urethra), or uncontrolled viral spread. Treatment may also be indicated for those who are at increased risk for severe disease, including those with weakened immune systems or some skin conditions such as eczema.
What should someone do if they think they have been exposed to someone with mpox?
In most cases, monkeypox is not a medical emergency, so patients should not go to the emergency department. Evaluation to determine if monkeypox testing is needed can be scheduled by contacting a primary care physician’s office or via urgent care clinics, usually as same day appointments. Patients with difficulty breathing, altered level of consciousness, decreased vision, uncontrollable pain or other severe mpox manifestations should seek medical care immediately.