School of Nursing eyes improving care, decreasing costs through care coordination
Collaborative research group looks to mobile technology tool
People with cancer and other chronic diseases face a complex care system. Complicated treatment regimens, multiple specialists with individualized therapies and a web of health care bureaucracy drive up cost and decrease quality in care. To address the negatives of fragmented care, poor communication and increasing expense, an interdisciplinary team from the Betty Irene Moore School of Nursing and the UC Davis Comprehensive Cancer Center launched the Collaborative Care Coordination Research Group to explore new models of nurse-directed, technology-enabled care coordination.
 As part of a team, nurses understand the role of providers, dynamics of family and knowledge of community to keep care centered on the individual who is receiving it.
As part of a team, nurses understand the role of providers, dynamics of family and knowledge of community to keep care centered on the individual who is receiving it.
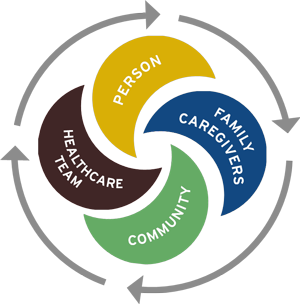
“As part of a team, nurses understand the role of primary providers, specialists, symptoms, quality of life, and knowledge of the community and the institution,” explained Jill Joseph, professor at the School of Nursing. “The center of that team is the person who is coming for care. We are focused on determining what the person needs, who can deliver it best and what will make the best-quality care, improve population health and cut down costs.”
The goal of coordinated care is to make sure people get the right care at right time and that all providers and family members are kept in the loop of the treatment plan. The approach, usually led by nurses, cuts down on duplication of services and reduces errors.
For example, one project examined two groups of people undergoing chemotherapy: half experienced coordinated care using technology, the other without it.
“Think of it as a private social network for cancer care. The person going through chemotherapy can have full access to the all the resources they need to partner with the health-care team through a tablet or computer,” said Katherine Kim, an assistant professor at the School of Nursing and member of the group.
The unique and private Personal Health Network is far more than an electronic health record. It is an ever-evolving collection of providers, family members, specialists, caregivers and educational resources in one place. Everyone, from hospital clinicians and holistic providers to local and long-distance family members, is connected.
“During chemotherapy treatment, people with cancer develop relationships with multiple care-team members who must also communicate with one another over time and across locations,” added Janice Bell, associate professor and another group member. “The person with cancer, providers and approved family members can be in the same group to keep the lines of communication open and provide one place for educational materials and real-time feedback.”
Disjointed care and weak communication are costly and can greatly increase the likelihood of hospitalization. A study by the Institute of Medicine estimates care coordination efforts could save as much as $240 billion annually. One member of the group, Robin Whitney, a graduate of the Nursing Science and Health-Care Leadership Doctor of Philosophy Degree Program, is a cancer survivor who understands the struggles.
“It was hard even as a registered nurse and educated person in health care to navigate the system. When I was not feeling well, it was hard to figure out how to get my medicine and my needs met,” Whitney said. “As a researcher, I love being involved in this attempt to improve care.”
“This hands-on preparation in getting research off the ground is a highly functional, collaborative, engaged and supportive experience,” added Sarah Reed, a social worker and graduate student researcher also in the doctoral program at the School of Nursing. “The promise of discovery is always looming and the discovery will be able to make things better.”
The National Institutes of Health estimates the overall cost of cancer in 2009 was $86.6 billion for direct medical costs. To curb expense and spur new care practices, the federal government now fines health-care facilities if a person is readmitted within 30 days of discharge. A Robert Woods Johnson report, “The Revolving Door: A Report on U.S. Hospital Readmissions,” noted “while hospitals are getting hit with Medicare penalties because they are the key venue of care, they do not own this issue alone. Everyone in the health care system does.” UC Davis research group members recognize effective care coordination can shut that revolving door.
"Cancer treatment is extremely complex involving different specialties, extending over a period of months to years and may be associated with significant side effects,” said Richard Bold, professor and chief of surgical oncology at the UC Davis Comprehensive Cancer Center. “These people are at high risk for adverse events, potentially leading to hospital admission. Coordination of care among all providers and the person with cancer may potentially minimize the impact of the side effects on their health. I am looking forward to see how this technology can impact care coordination of those facing these complex, challenging situations."
While this School of Nursing-led research group initially focused on cancer, other research projects are now underway. Professors partnered with a network of Central Valley primary-care centers to train nurses and medical assistants to serve as health coaches. Another study aims to develop technology for a personal health network to enhance early palliative care for older adults. Professors and graduate research assistants are also looking to the role technology can play to create a network connecting UC clinics to other health centers.
“The end goal is the School of Nursing provides a model of care that can be disseminated and applied to multiple conditions to meet the triple aim: care, health and cost,” Joseph added. “Our work impacts many health conditions, provides a venue for education and training, and demonstrates credibility for the research our faculty and students conduct on a daily basis.”
The video below showcases the work of these Betty Irene Moore School of Nursing researchers in the use of mobile technology and cancer care coordination.
Collaborative Care Coordination Research Group Publications
Predictors of financial difficulties and work modifications among cancer survivors in the United States.
Whitney RL, Bell JF, Reed SC, Lash R, Bold RJ, Kim KK, Davis A, Copenhaver D, Joseph JG
2015/2016
Systematic Review of Emergency Department Use Among Cancer Patients.
Lash RS, Bell JF, Reed SC, Poghosyan H, Rodgers J, Kim KK, Bold RJ, Joseph JG
2016
Personal Health Network for Chemotherapy Care Coordination: Evaluation of Usability Among Patients.
Kim KK, Bell JF, Bold R, Davis A, Ngo V, Reed SC, Joseph JG
2016
Mobile Care Coordination System for the Management of Complex Chronic Disease.
Haynes S, Kim KK
2016
Systematic Review of Hospital Readmissions among US Patients with Cancer
Bell JF, Whitney RL, Reed SC, Poghosyan H, Lash R, Kim KK, Davis A, Bold RJ, Joseph JG
Health Care Quality Experiences Among Cancer Survivors In The United States
Bell J, Whitney RL, Reed S, Davis A, Kim K, Copenhaver D, et al
2014
Development And Implementation Of A Novel Personal Health Network Technology For Cancer Care Coordination
Bell J, Kim K, Davis A, Reed, S, Bold R, Cerrone K, Altobello A, Homchowdhury J, Joseph J
2014
Psychosocial Outcomes In Active Treatment Through Survivorship. ASCO Annual Meeting Proceedings
Reed SC, Bell J, Whitney RL, Davis A, Lash RS, Kim K, et al
2014
Work And Financial Disparities Among Adult Cancer Survivors In The United States
Whitney RL, Bell J, Reed S, Davis A, Lash RS, Kim K, et al
2014
A Framework For Person-Centered, Community-Wide Care Coordination
Kim KK, Bell JF, Boicey CM, Freeman-Daily J, McCollister-Slipp, Joseph, JG
2015
Parenting Experiences Of Cancer Survivors With Young Children In The 2012 LIVESTRONG Survey For People Affected by Cancer
Whitney RL, Bell J, Reed SC, Blackmon E, Kim KK, Joseph JG
2016
Caregiver Work Modifications: A Hidden Cost Of Cancer Care
Blackmon E, Bell J, Whitney RL, Reed SC, Kim K, Joseph J
2016
Psychosocial Outcomes Among Cancer Survivors Who Receive A Treatment Summary Or Survivorship Care Plan
Reed SC, Bell J, Whitney RL, Blackmon E, Kim KK, Joseph JG
2016
Mobile Technology For Cancer Care Coordination: Exploring Usability And Acceptance
Morgan J, Bell JF, Kim KK, Ngo V, Joseph JG
2016
Usability And Acceptance Of Novel Personal Health Technology To Support Early Palliative Care For Patients With Cancer And Caregivers
Bell JF, Reed SC, Kim KK, Ngo V, Wait W, Apesoa-Varano E, Morgan J, Whitney RL, Blackmon E, Jill Joseph
2016